This document provides an overview of vasculitis, including:
- Vasculitis refers to inflammation of blood vessel walls and can range from mild to life-threatening.
- It encompasses a large group of diseases characterized by inflammatory reactions in blood vessel walls. The causes are often unknown but can be triggered by various stimuli.
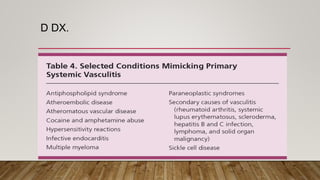
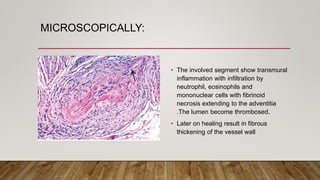
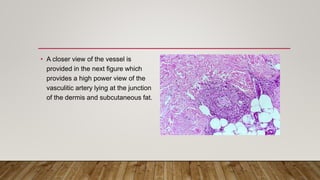
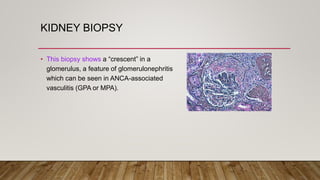
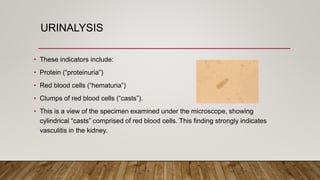
- Diagnosis involves blood tests, biopsies of affected tissues like skin and kidneys, and imaging tests. Biopsies examined under a microscope are often needed to confirm a diagnosis of vasculitis.
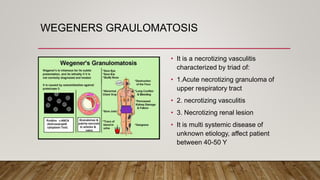
![ANCA ASSOCITED DS.
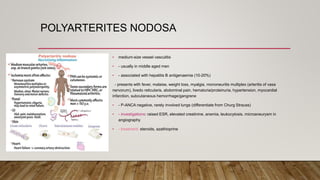
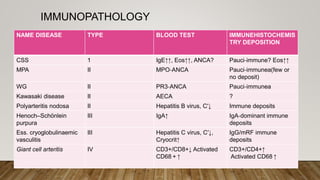
• ANCA tests — ANCA is an abbreviation (acronym) for anti–neutrophil cytoplasmic
antibodies. These antibodies are found in the blood of patients with several different
types of vasculitis, including Wegener’s Granulomatosis, Microscopic Polyangiitis,
and the Churg–Strauss Syndrome.
• ANCAs are detected by a simple blood test. These antibodies are directed against the
cytoplasm (the non–nucleus part) of white blood cells.
• ANCAs come in two primary forms:
• 1) the C–ANCA [C stands for cytoplasmic].
• 2) the P–ANCA [P stands for perinuclear].](https://image.slidesharecdn.com/vasculitis-210702134625/85/Vasculitis-26-320.jpg)