This document provides an overview of vasculitis, including:
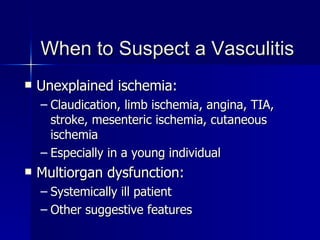
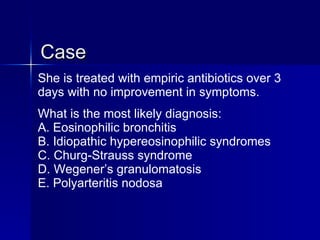
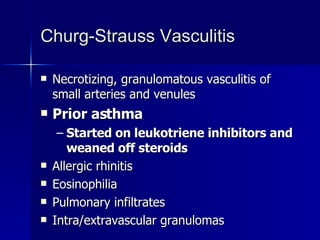
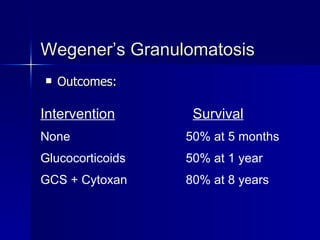
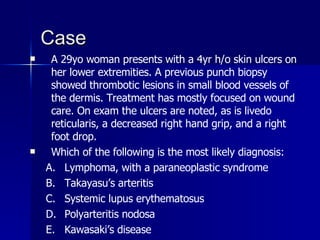
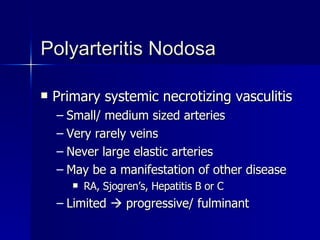
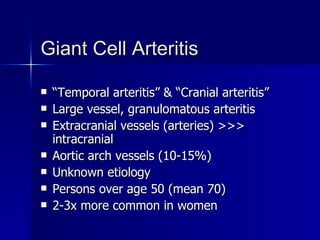
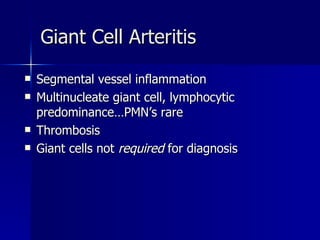
1) Vasculitis is inflammation and necrosis of blood vessels that can lead to occlusion, ischemia, and multi-system organ dysfunction.
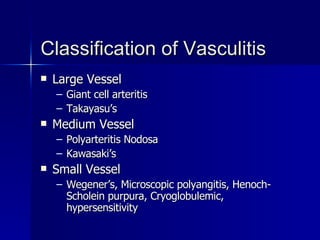
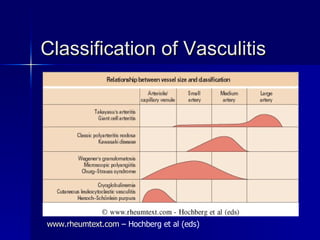
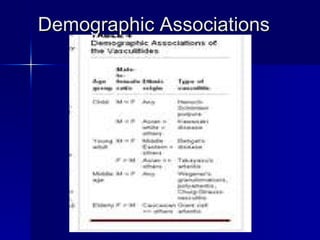
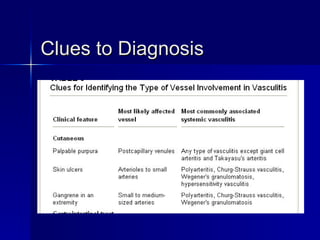
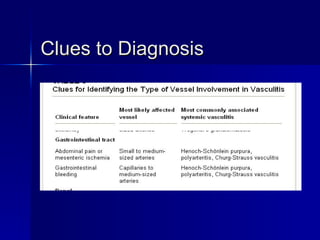
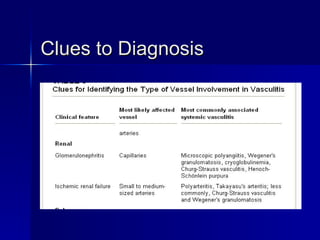
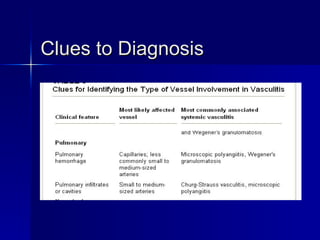
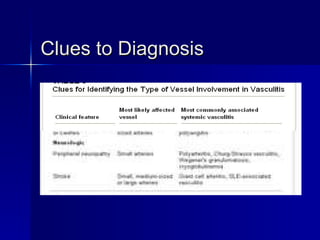
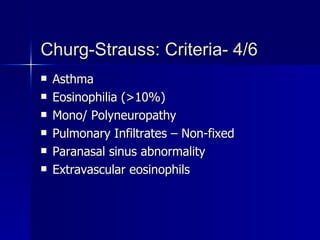
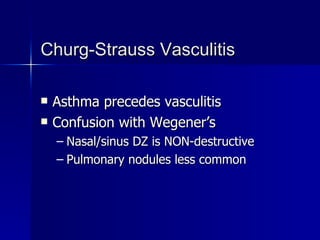
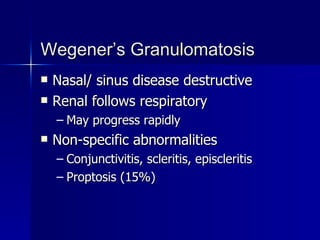
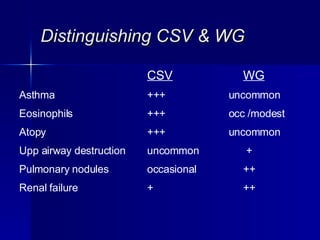
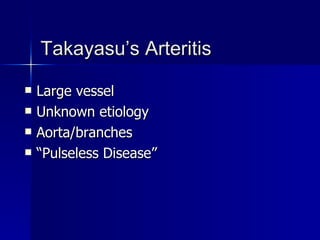
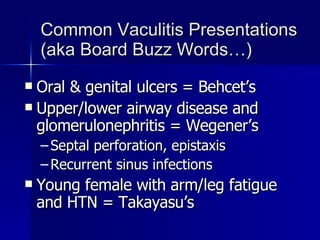
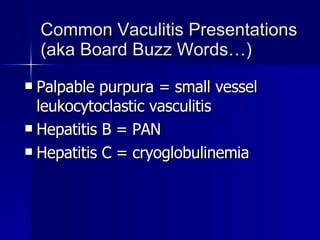
2) It is classified based on the size of affected vessels as well as the organ systems involved.
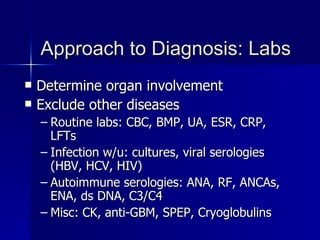
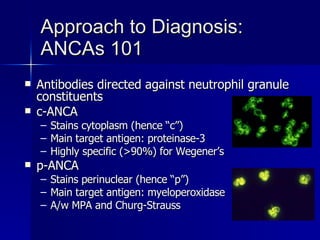
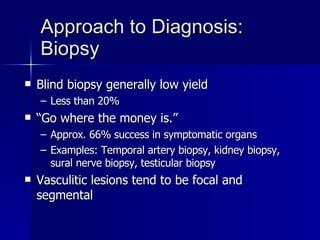
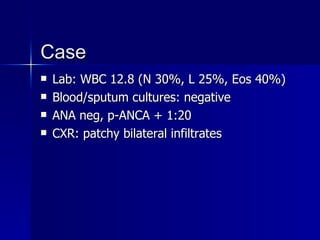
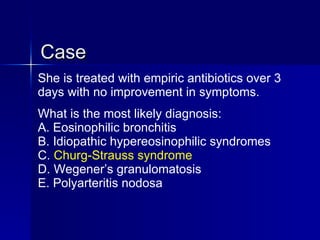
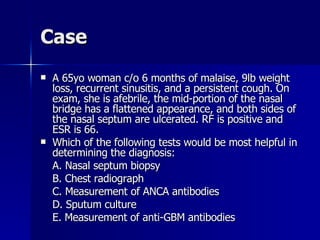
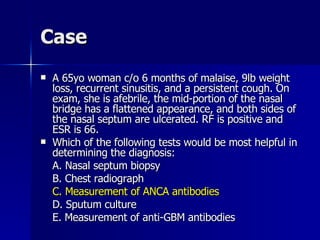
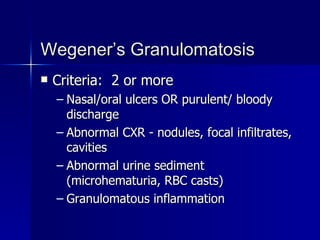
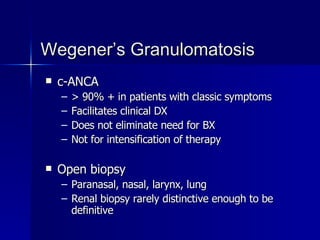
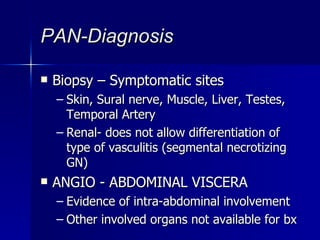
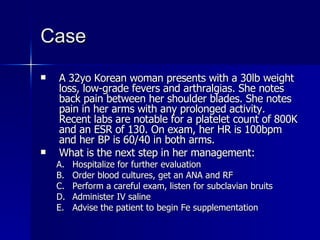
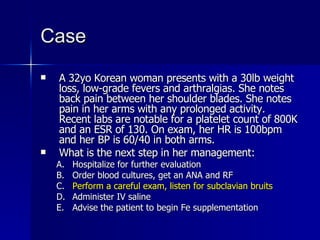
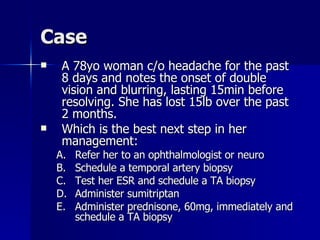
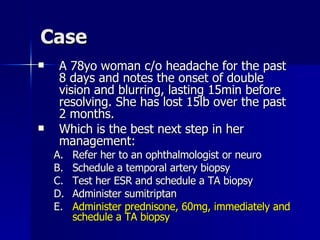
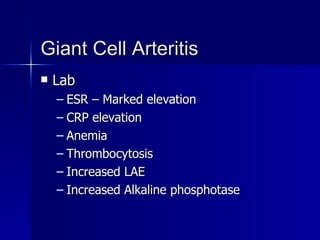
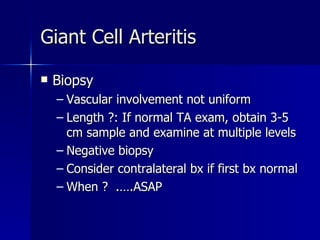
3) Diagnosis involves determining which organ systems are affected, excluding other potential causes, and obtaining biopsies of involved tissues when possible. Laboratory tests including ANCA can also provide clues to diagnosis.