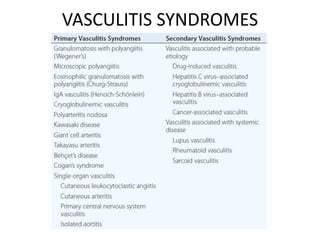
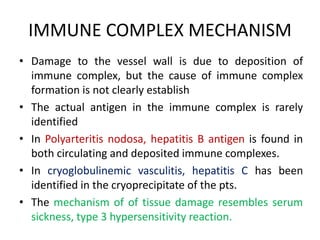
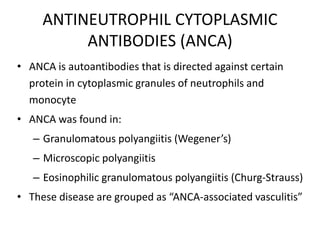
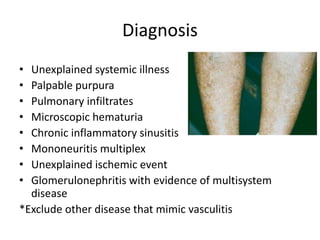
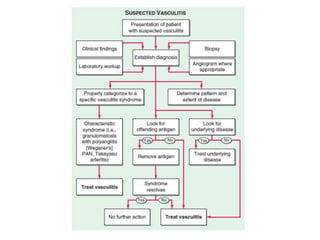
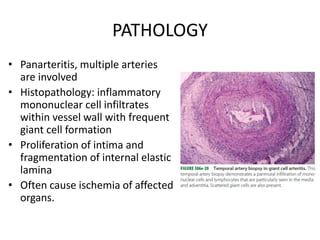
Vasculitis refers to inflammation of blood vessels. This document discusses the classification, pathogenesis, and syndromes of vasculitis. It is difficult to classify vasculitis due to overlapping features and unknown causes. The Chapel Hill system divides vasculitis by vessel size. Mechanisms include immune complex formation, ANCA production, and T-cell responses. Large vessel vasculitis includes giant cell arteritis and Takayasu arteritis. Giant cell arteritis causes headaches and vision loss. Treatment is glucocorticoids. Takayasu arteritis causes reduced pulses and organ ischemia, especially in young Asian women. Both can lead to complications like aneurysms if untreated.