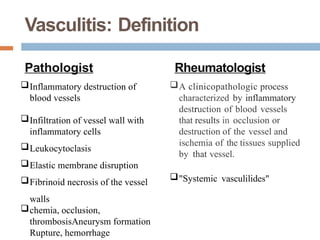
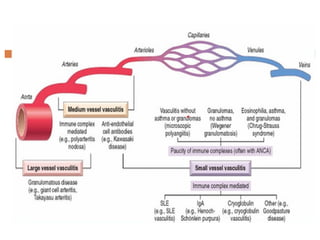
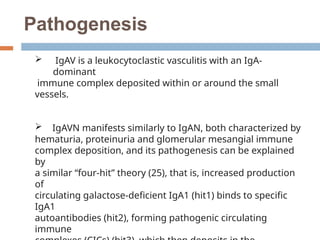
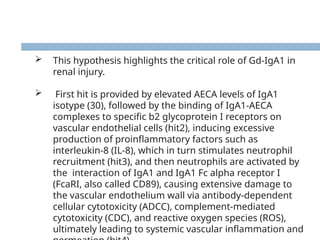
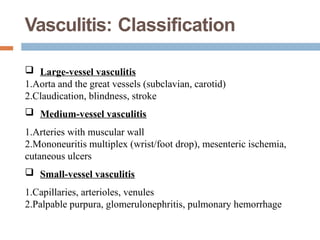
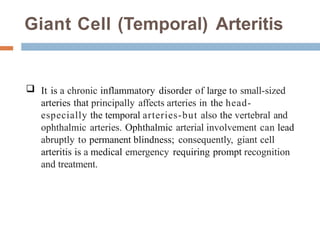
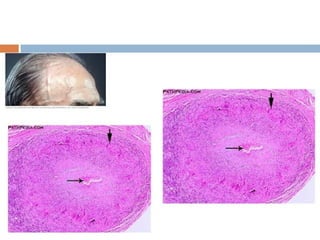
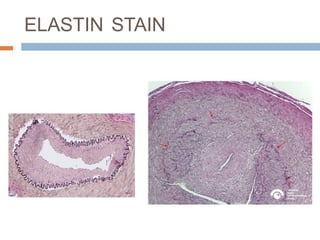
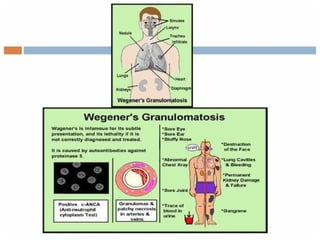
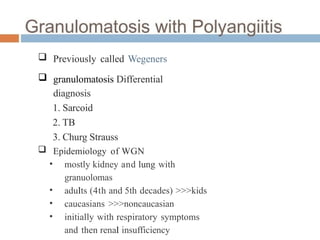
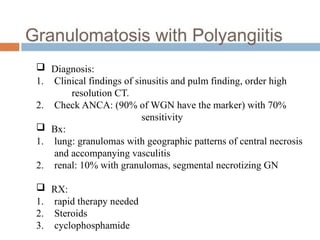
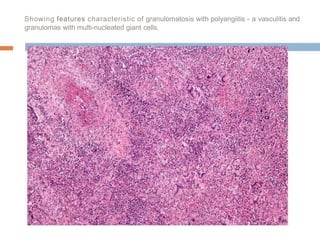
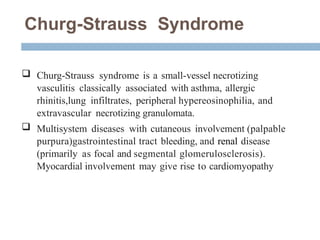
Vasculitis is a group of diseases characterized by inflammation of blood vessels, affecting various types and sizes across different organs, with common causes including immune-mediated mechanisms and infections. It is classified into large, medium, and small-vessel vasculitis with varying symptoms and clinical features, necessitating prompt recognition and treatment to prevent complications. Management strategies depend on disease severity and can include glucocorticoids and other targeted agents, though challenges in effective treatment persist due to limited high-quality data.