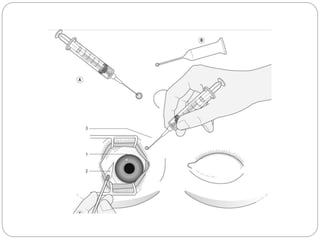
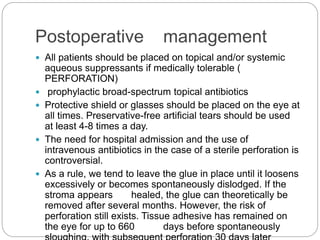
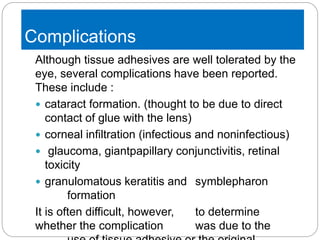
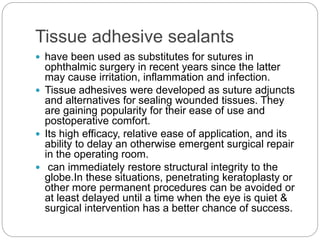
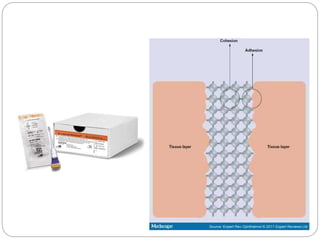
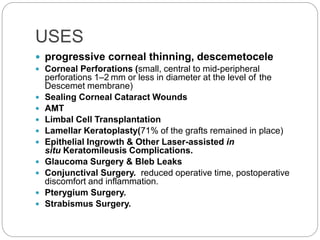
Tissue adhesives are increasingly being used as an alternative to sutures in ophthalmic surgery due to their ease of use and reduced postoperative discomfort. The document discusses various types of tissue adhesives including synthetic cyanoacrylate derivatives and biologic fibrin-based adhesives. It provides details on the uses of tissue adhesives in conditions like corneal thinning, perforations, and glaucoma surgery. Application techniques and postoperative management are also outlined. While well-tolerated, potential complications including infection, infiltration, and cataract formation are noted.
![ Sharma et al. compared the effectiveness of fibrin
glue and N-cyanoacrylate for treating small
corneal perforations of 3 mm diameter.[20]Both
adhesives resulted in effective closure of corneal
perforations <3 mm in diameter. The investigators
demonstrated that adhesive plug formation with
cyanoacrylate was faster than that of fibrin glue.
However, fibrin glue-assisted corneal perforation
closure resulted in faster healing and less
vascularization.](https://image.slidesharecdn.com/glue-190802090703/85/Tissue-Adhesive-In-Ophthalmology-9-320.jpg)