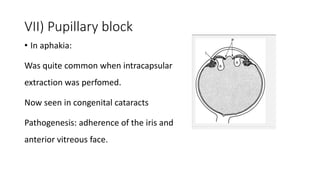
This document discusses glaucoma that can occur after cataract surgery (aphakia and pseudophakia). It defines the terms and outlines the incidence of glaucoma after different types of cataract surgery procedures. Various mechanisms by which cataract surgery can lead to glaucoma are described, including effects of viscoelastic substances, inflammation, pigment dispersion, angle distortion, pupillary block, and steroid use. Precautions during surgery and management approaches for early and late post-operative glaucoma are provided. Trabeculectomy is the preferred surgical treatment if maximum medical therapy fails to control glaucoma in these cases.