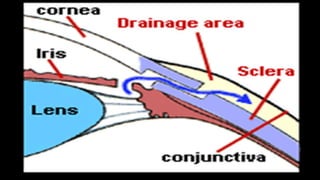
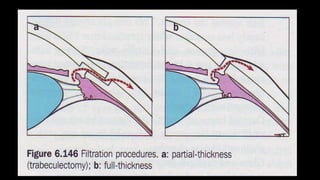
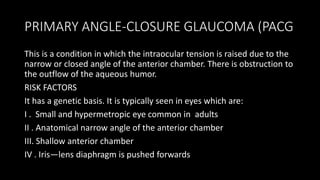
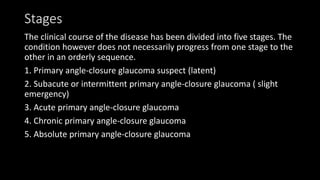
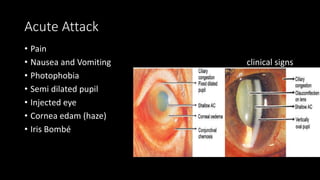
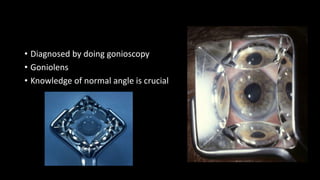
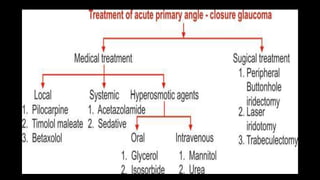
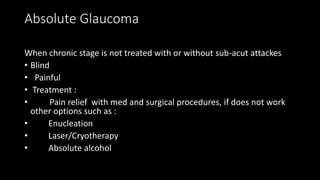
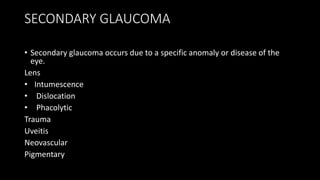
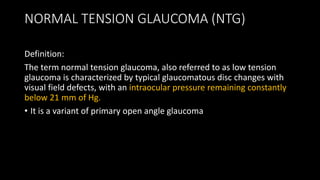
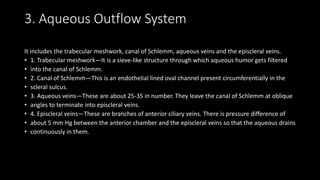
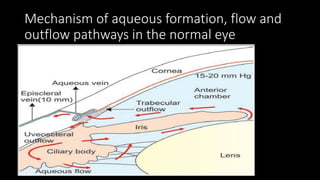
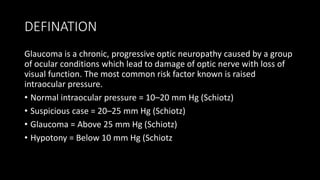
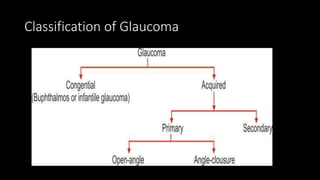
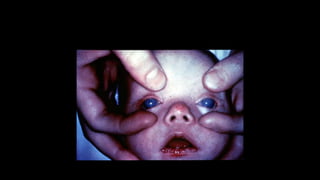
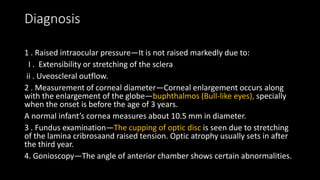
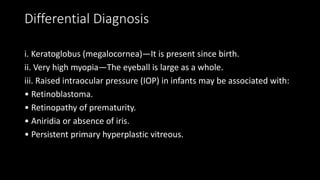
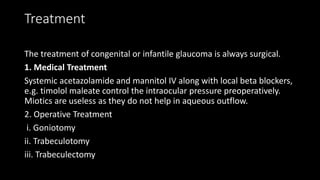
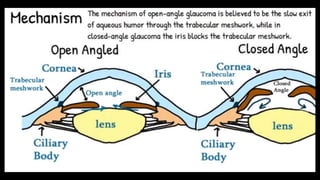
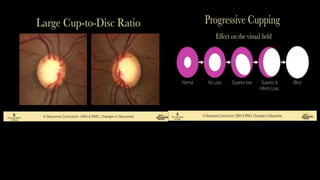
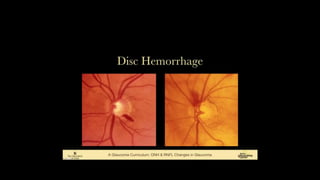
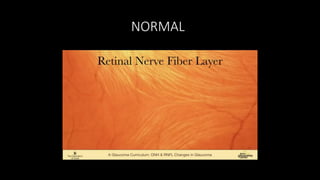
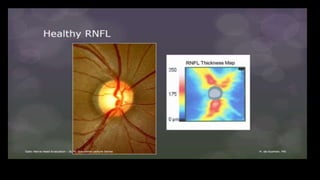
The document covers glaucoma, detailing its anatomy, physiology, types, pathogenesis, symptoms, diagnosis, and treatment. It explains various classifications, including congenital glaucoma, primary open angle glaucoma, and angle-closure glaucoma, highlighting their etiologies and clinical presentations. Treatment options range from medical therapies to surgical interventions depending on the specific type and severity of glaucoma.


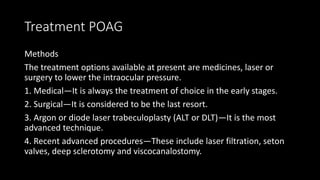
![Treatment POAG
• β-blockers (Timolol)
• Parasympathomimetics [Miotics] (Pilocarpine)
• Carbonic Anhydrase inhibitors (Dorzolamide)
• Adrenergic Agonists (Dipivefrin, Brimonidine)
• Prostaglandin analogues (Latanoprost)
• Hyperosmotic Agents (Mannitol, Glycerine, Isosorbide)](https://image.slidesharecdn.com/glaucoma-211211142509/85/Glaucoma-40-320.jpg)