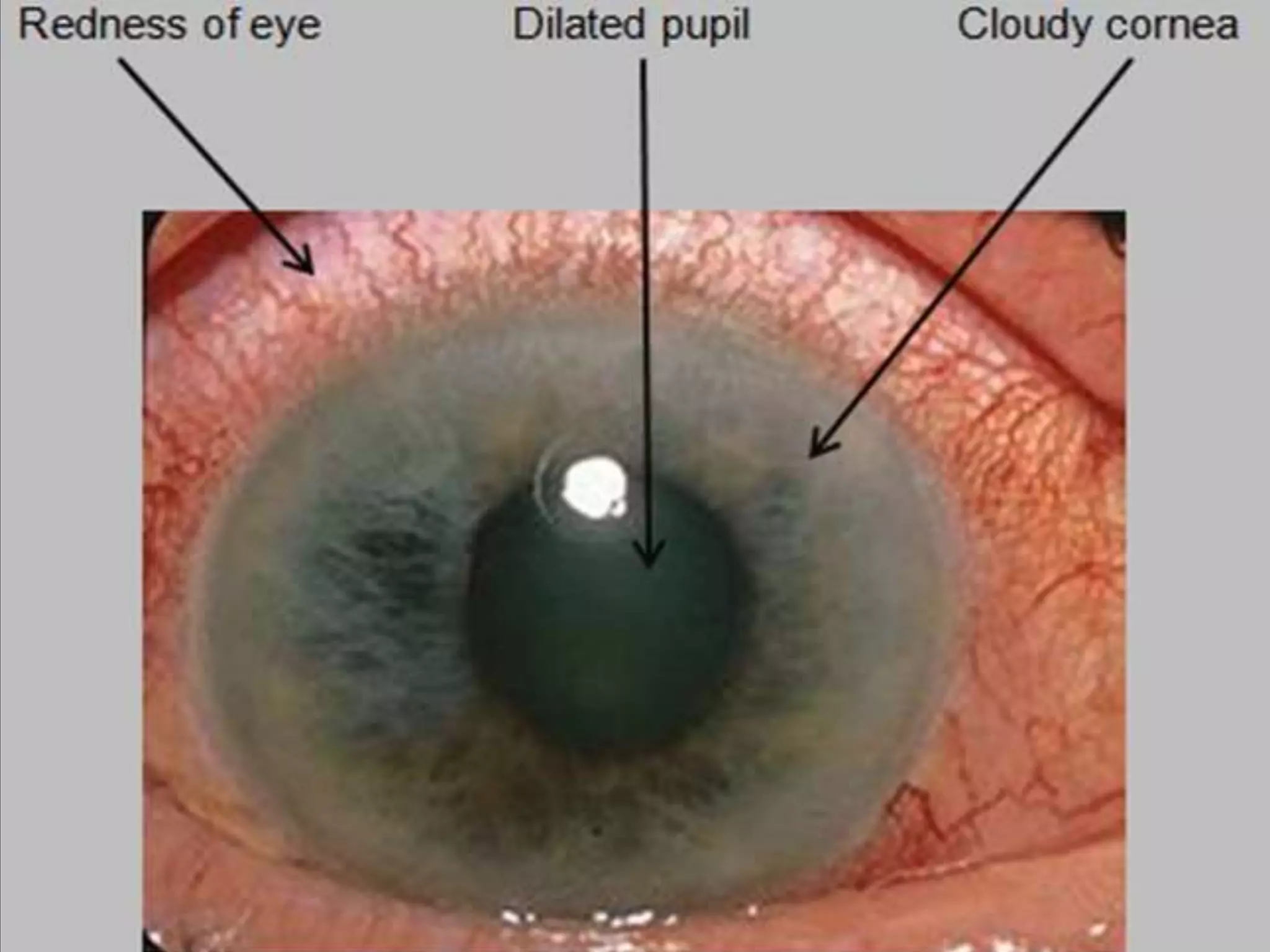
Acute congestive glaucoma is a medical emergency characterized by increased intraocular pressure due to blockage of aqueous humor outflow, often affecting individuals of Far Eastern and Indian Asian descent. Risk factors include age, gender, race, and anatomical features of the eye. Management involves hospitalization, medication to lower intraocular pressure, and potential surgical interventions such as peripheral iridotomy.























![Treatment
• Hospitalization :patient should assume a supine position to
encourage the lens to shift posteriorly under the influence of
gravity.
Systemic Treatment :
• IV Acetazolamide((Diamox)) [C/I sulfonamide allergy]
• IV mannitol [Circulatory overload C/I in heart failure]
Topical Treatment
• M3 agonist( Pilocarpine) → Miosis→ (↓IOP)
• β-blocker (Timolol ) → ↓AH syn. → (↓IOP)
• α2-agonist( Apraclonidine) → ↓A.H. syn. → (↓IOP)
• Topical steroids for inflammation
• Analgesia and an Antiemetic may be required
• peripheral Iridotomy or iridectomy
• Prophylactic iridotomy or iridoectomy to other eye](https://image.slidesharecdn.com/acutecongestiveglaucoma-181231205604/75/primary-closed-angle-glaucoma-Acute-congestive-glaucoma-29-2048.jpg)


