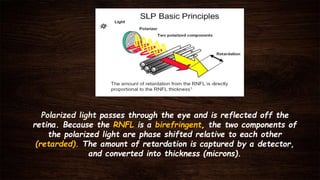
This document provides an overview of the GDx scanning laser polarimetry device used to measure retinal nerve fiber layer (RNFL) thickness. It discusses how GDx works by measuring the birefringence of the RNFL using polarized light. GDx provides high sensitivity (89%) and specificity (98%) in detecting glaucoma. RNFL assessment is important because damage occurs earlier than visual field or optic nerve head changes. GDx outputs include RNFL thickness maps, deviation maps, and TSNIT parameters to analyze RNFL structure and detect loss. It can detect glaucoma earlier than visual fields and helps monitor for progression.