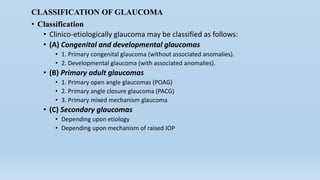
Glaucoma is a group of eye diseases characterized by optic nerve damage and visual field loss. It is often associated with elevated intraocular pressure but can sometimes occur with normal pressures. The two main types are open-angle glaucoma and angle-closure glaucoma. Congenital glaucoma is present at birth and results from impaired aqueous outflow, often due to developmental abnormalities in the trabecular meshwork. It is typically treated surgically through procedures like goniotomy or trabeculotomy to improve drainage and lower pressure. Long term monitoring is important as the disease can progress if not properly managed.