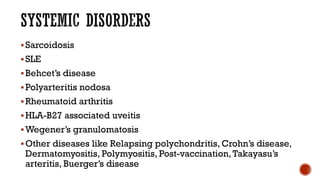
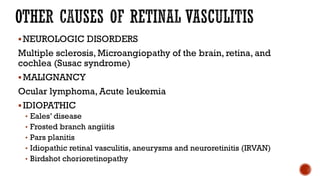
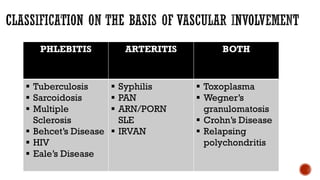
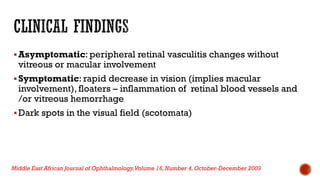
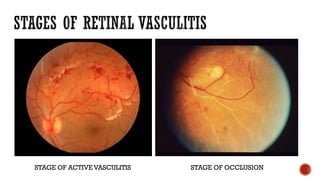
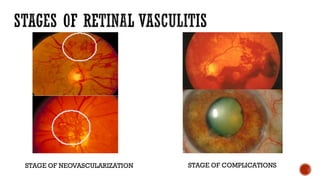
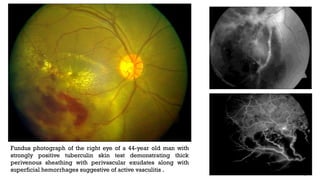
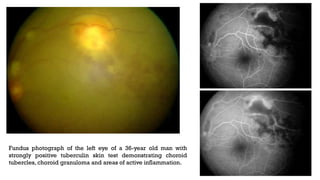
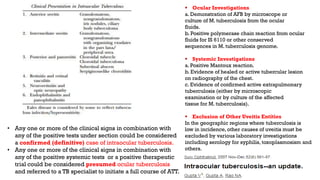
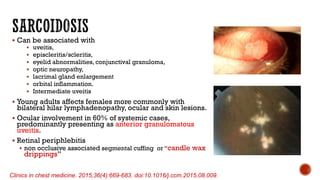
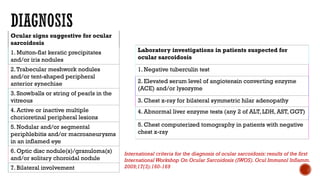
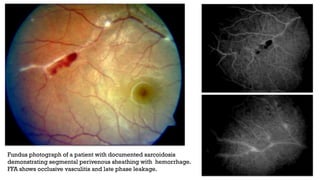
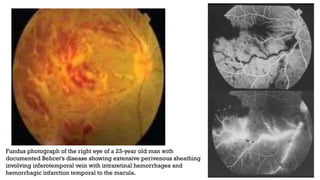
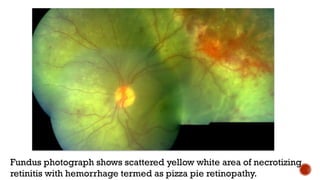
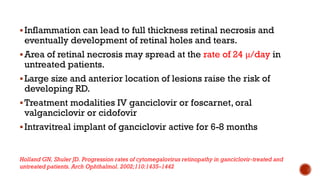
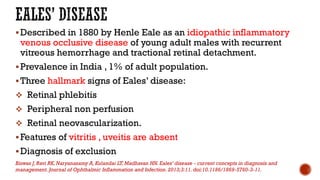
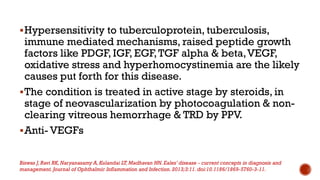
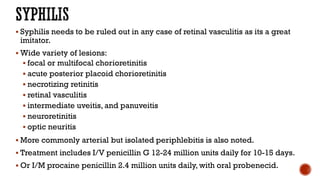
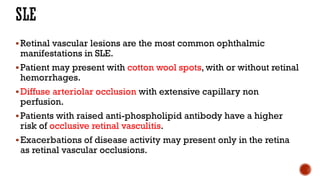
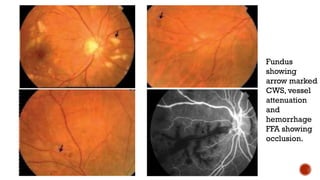
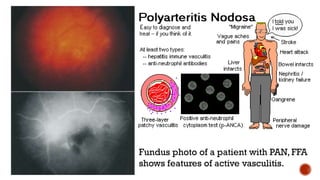
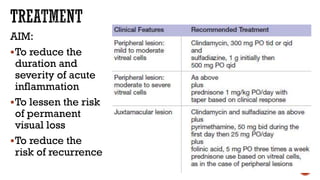
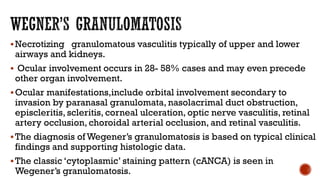
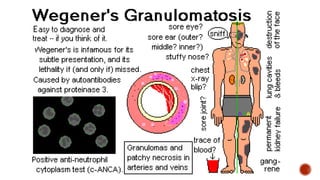
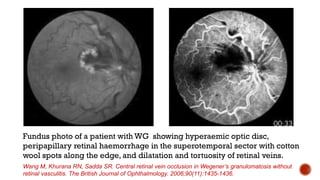
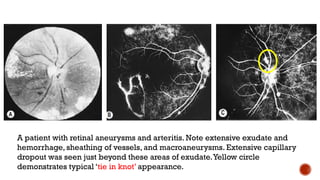
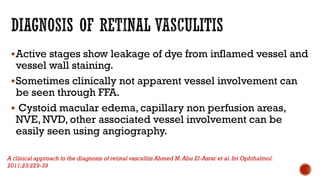
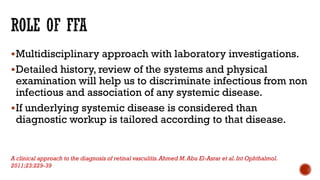
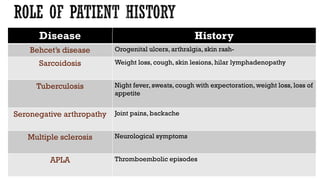
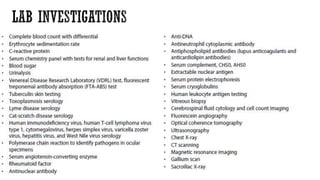
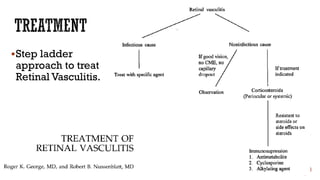
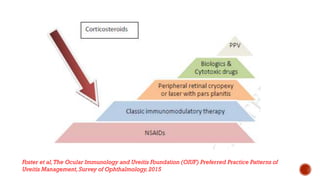
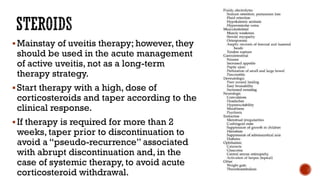
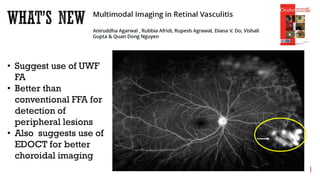
The document discusses various forms of retinal vasculitis and its underlying causes, including infectious, systemic, neurological, and idiopathic factors. It highlights the diagnostic challenges and treatment options for ocular conditions such as tuberculosis, sarcoidosis, and Behçet's disease, emphasizing the significance of accurate diagnosis in managing ocular inflammation. Additionally, it outlines the clinical manifestations, diagnostic criteria, and therapeutic approaches for different types of uveitis associated with these conditions.