This document discusses macular holes (MH), including their history, pathogenesis, classification, diagnosis, and treatment. Some key points:
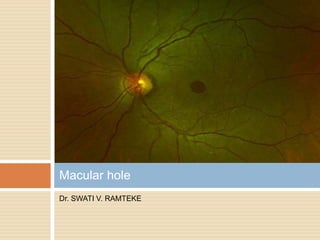
- MH are round openings in the foveal center that were first described in 1869. Vitreomacular traction is a leading hypothesis for their pathogenesis.
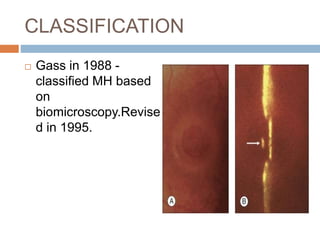
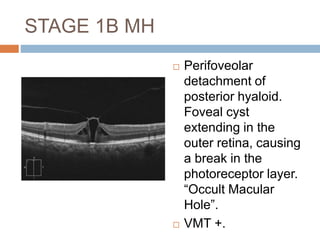
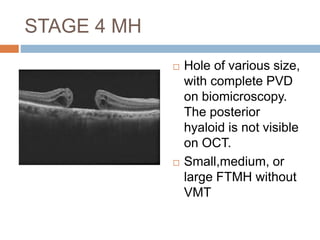
- MH are classified based on size and vitreous attachment status, ranging from stage 1 (impending) to stage 4 (full thickness hole with posterior vitreous detachment).
- Diagnosis involves biomicroscopy, OCT for staging, and fellow eye screening. Treatment involves pars plana vitrectomy to relieve traction, internal limiting membrane peeling, and gas/oil tamponade depending on