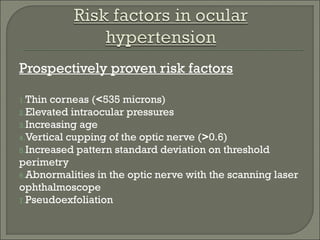
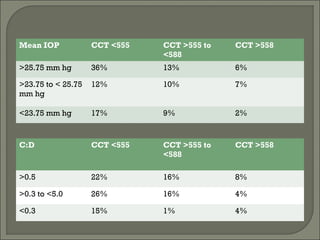
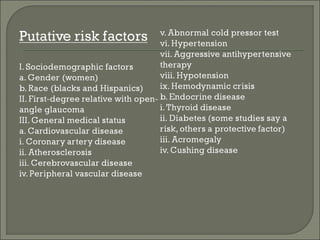
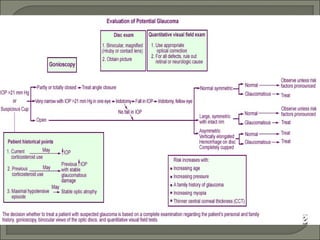
This document summarizes information about ocular hypertension (OHT) and glaucoma risk factors. It finds that 9.5% of patients with OHT developed glaucoma within 5 years without treatment, compared to 4.4% of treated patients. Thin corneas, elevated intraocular pressure, increasing age, optic nerve cupping, and visual field defects increase glaucoma risk. For OHT patients, a 20% IOP reduction can delay or prevent glaucoma, but most low-risk OHT patients can be monitored without medication, while high-risk patients may benefit from more frequent exams and early treatment based on their age, health, life expectancy, and preferences.