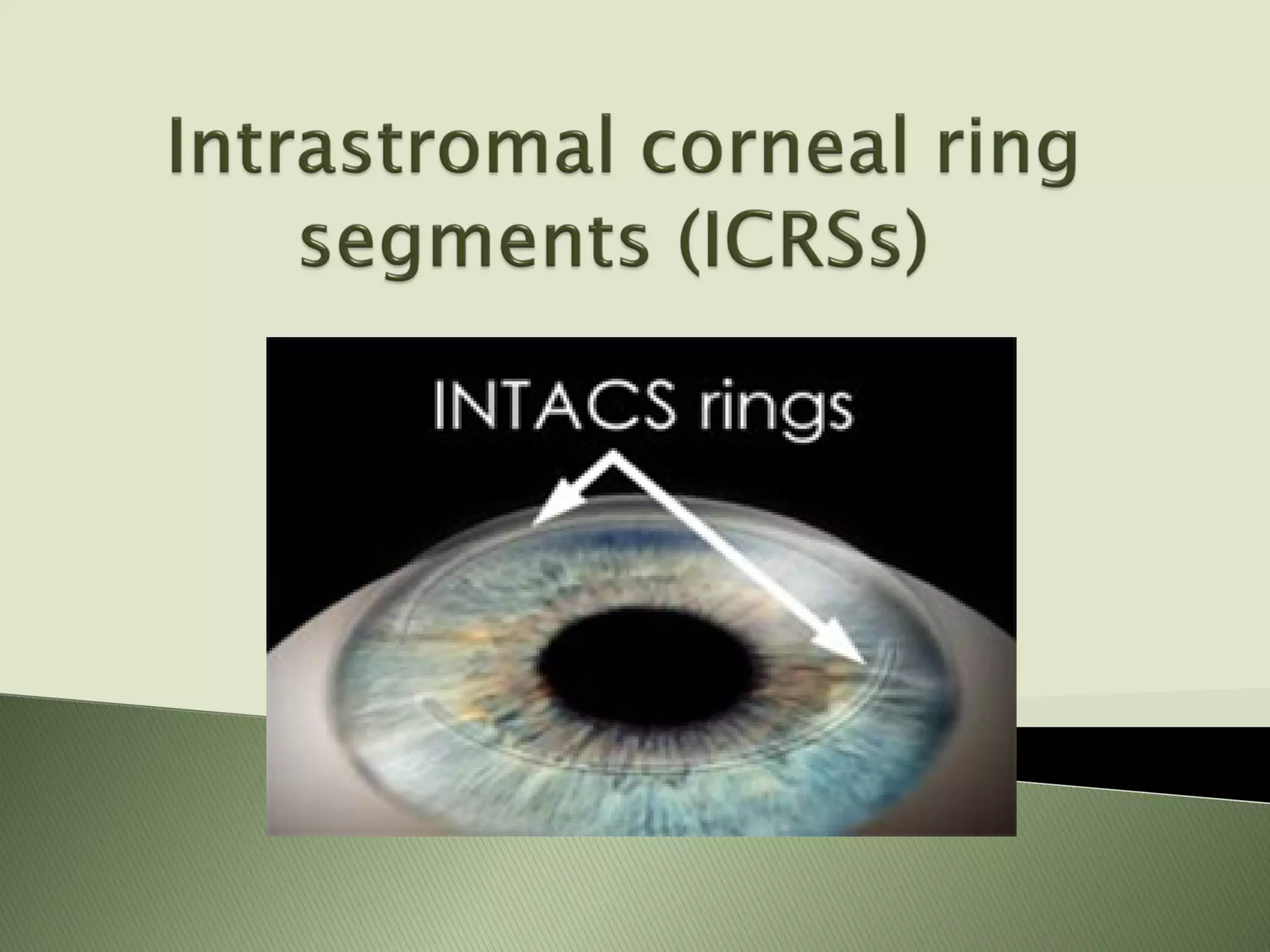
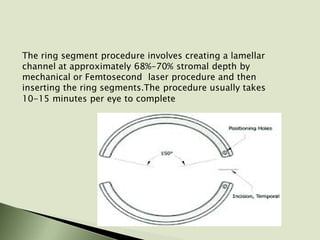
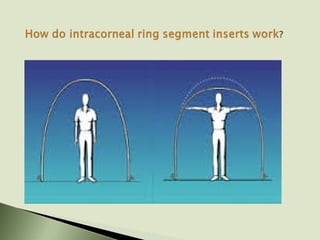
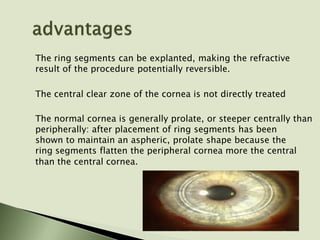
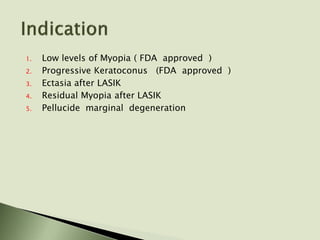
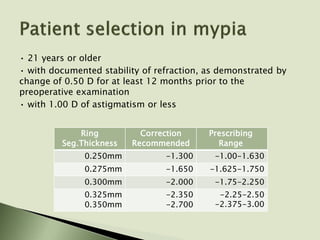
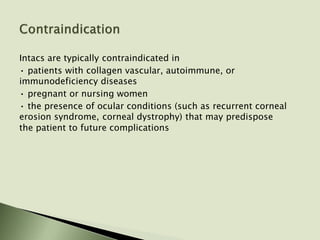
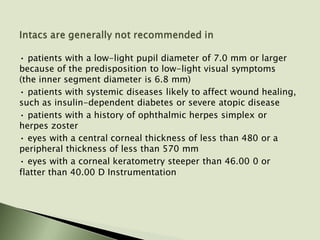
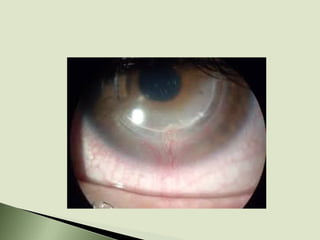
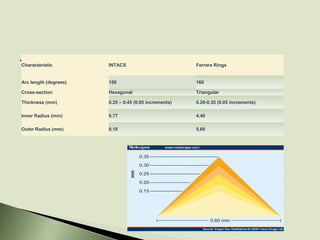
Intracorneal ring segments, such as INTACS, are thin plastic rings that are implanted into the corneal stroma to flatten the cornea and reduce myopia. They are placed in a lamellar channel using either a mechanical or laser procedure. Thicker rings provide greater flattening and myopia correction. Potential risks include visual disturbances and complications requiring removal. Intracorneal rings have been used off-label to treat conditions like post-LASIK ectasia and keratectasia with some success in improving vision.