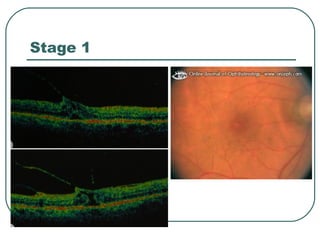
This document summarizes macular hole formation and treatment. It describes the stages of macular hole development classified by Gass. Vitrectomy surgery involving fluid-gas exchange has been shown to successfully reattach the macula and improve vision in 58-73% of cases. The author reports high success rates for macular hole closure and visual improvement with vitrectomy using various tamponades and adjuncts like internal limiting membrane peeling. Face down positioning after surgery is important for compliance and optimal outcomes.