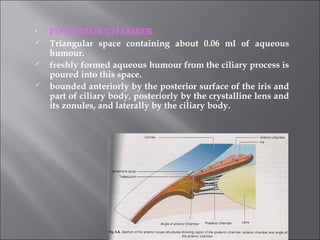
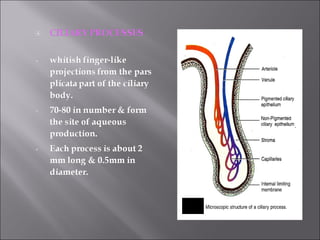
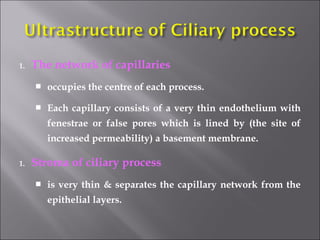
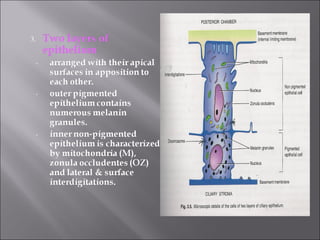
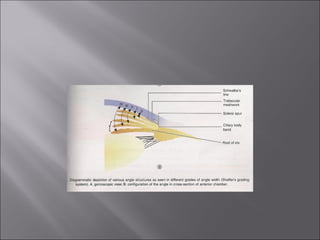
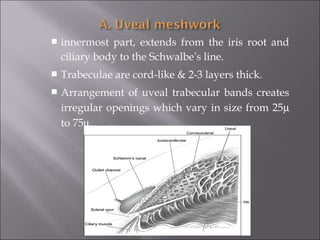
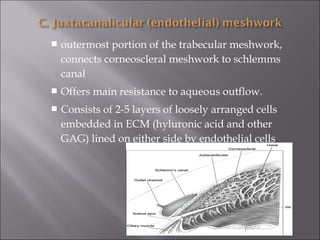
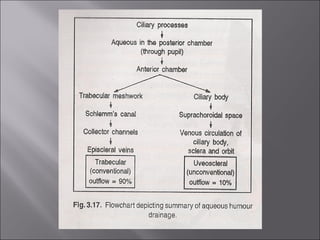
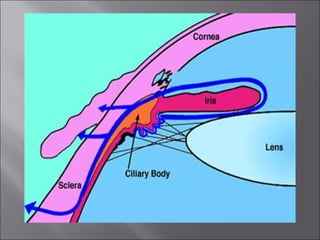
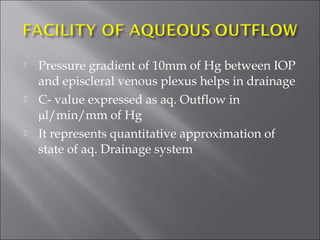
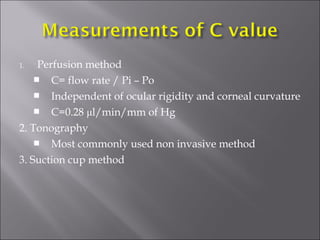
The document discusses the anatomy and physiology of aqueous humor in the eye. It describes how aqueous humor is continuously produced by the ciliary processes at a rate of 2.6-2.8 μl/min and circulates from the posterior chamber to the anterior chamber before draining out of the eye. Aqueous humor is formed primarily via active transport processes across the non-pigmented ciliary epithelium, establishing an osmotic gradient that allows fluid movement. It then drains from the anterior chamber through both the trabecular meshwork into Schlemm's canal and the uveoscleral pathway. The facility of aqueous outflow is represented by the C-value which is used to evaluate aqueous drainage and diagnose