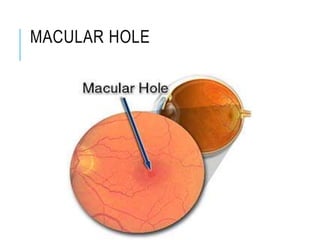
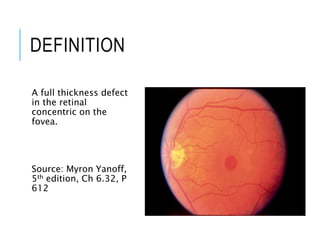
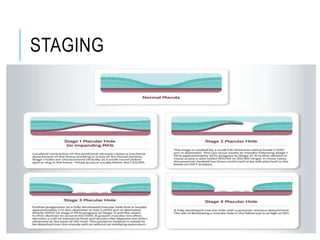
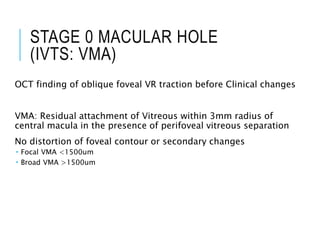
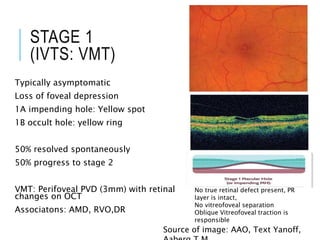
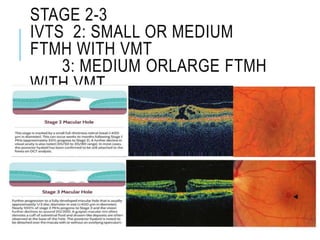
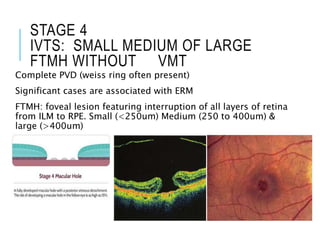
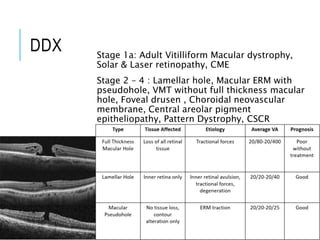
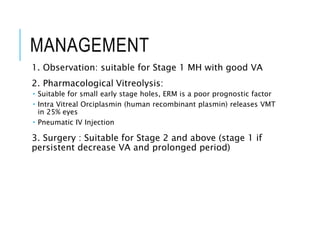
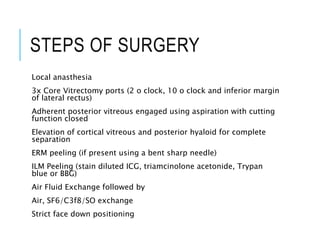
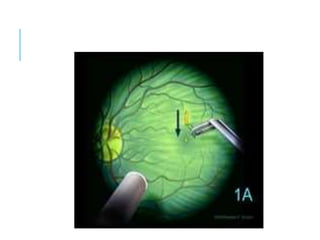
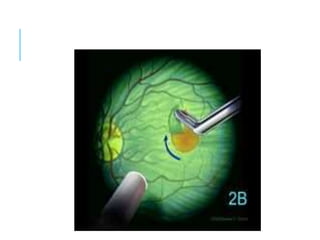
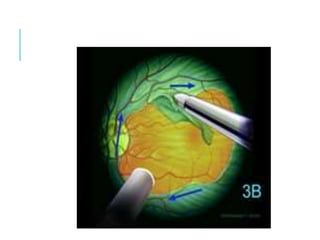
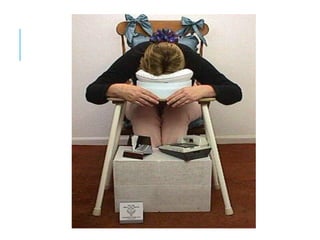
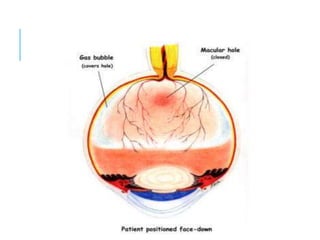
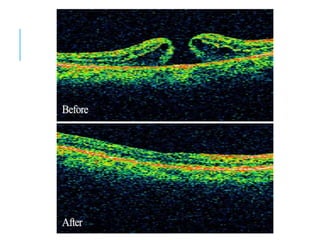
Macular holes are full thickness defects in the retina at the macula. Most are idiopathic and occur in older females. Vitreomacular traction causes focal shrinkage of the vitreous cortex at the fovea. Left untreated, macular holes may enlarge and visual acuity may decrease. Staging is based on optical coherence tomography findings, from vitreomacular adhesion to small, medium, and large full-thickness macular holes. Surgery involves vitrectomy with internal limiting membrane peeling and gas tamponade, followed by facedown positioning. This closes the hole in most cases, though complications can include cataract and retinal detachment.