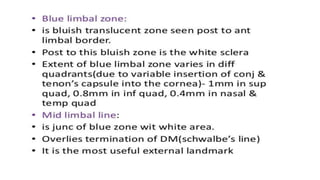
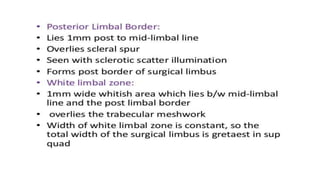
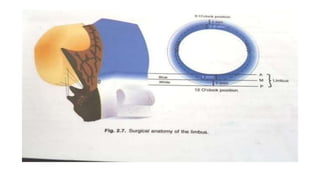
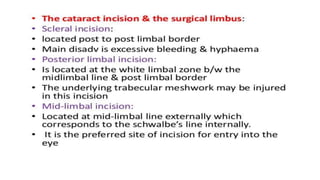
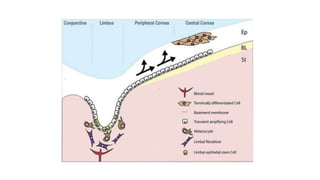
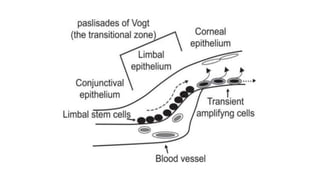
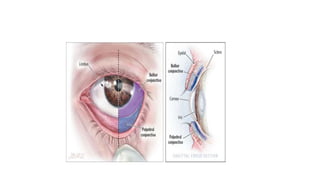
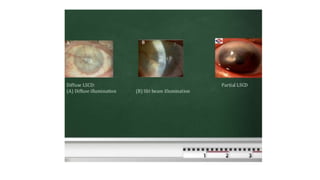
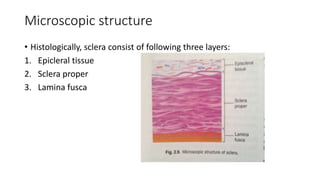
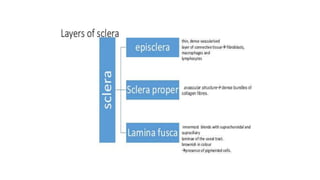
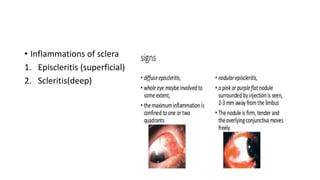
The limbus serves as the junction between the cornea and sclera, facilitating aqueous humor outflow and hosting stem cells essential for corneal epithelium renewal. Limbal epithelial stem cell deficiency can lead to serious corneal issues, necessitating grafting or alternative stem cell therapies for repair. The sclera encases the eyeball, providing structural support and attachment for muscles, and is composed of three layers with vascular and nerve supplies that contribute to its function and sensitivity to inflammation.