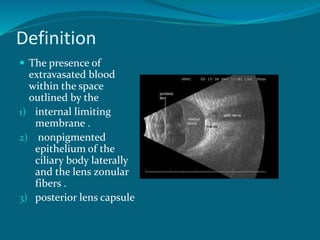
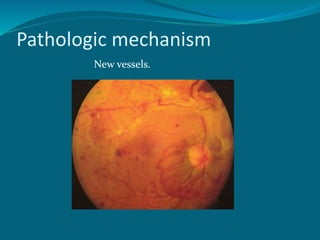
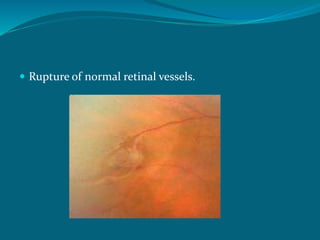
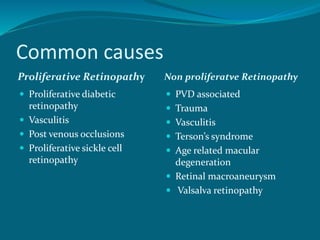
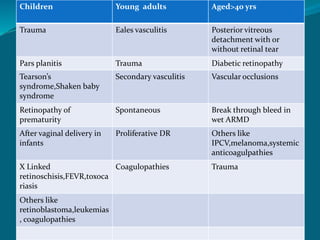
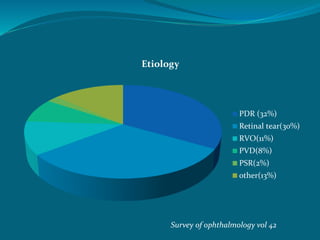
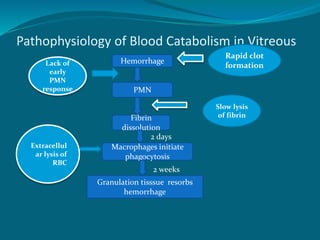
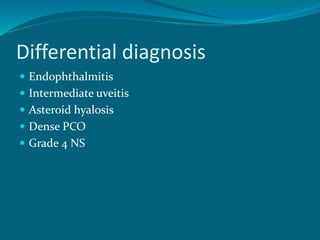
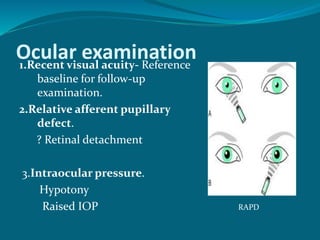
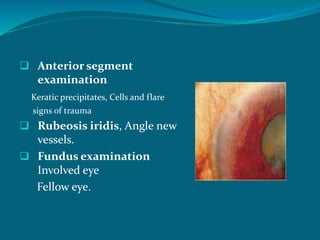
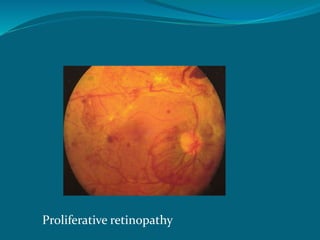
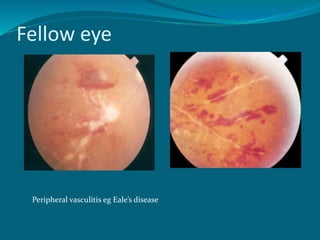
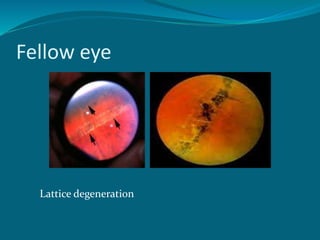
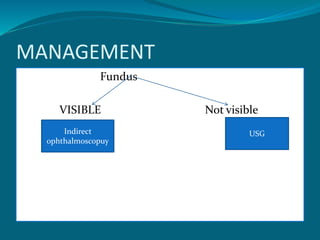
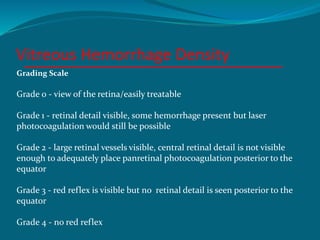
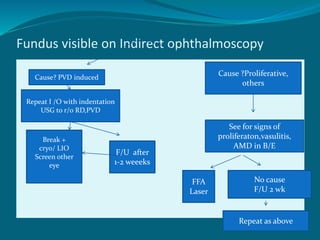
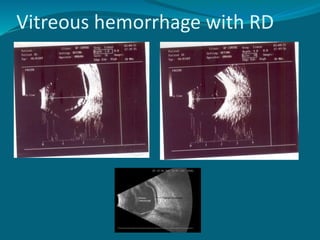
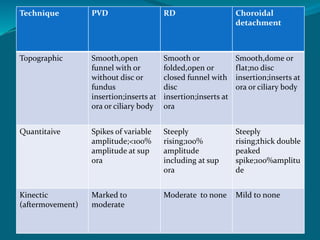
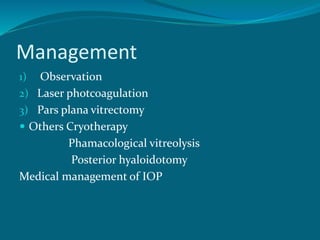
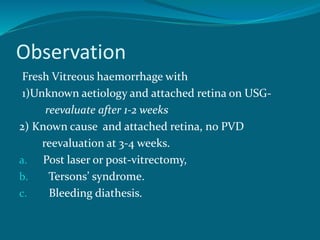
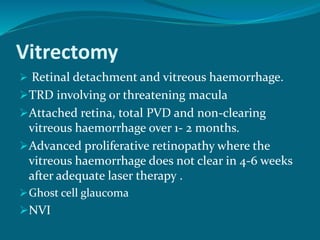
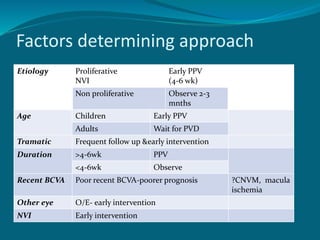
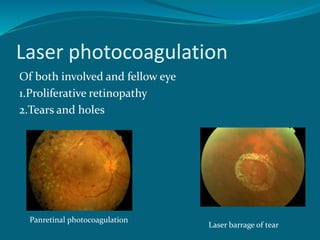
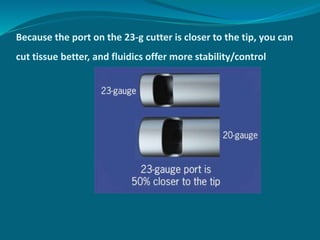
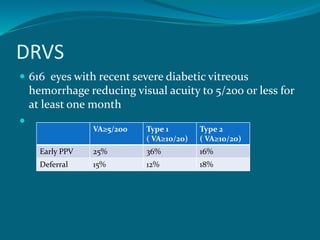
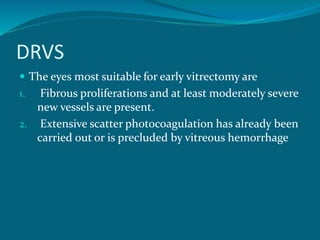
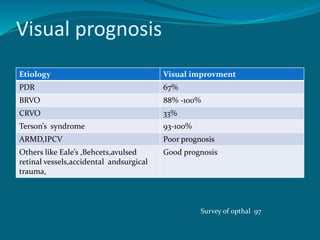
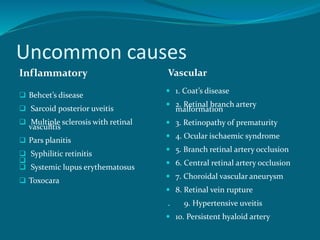
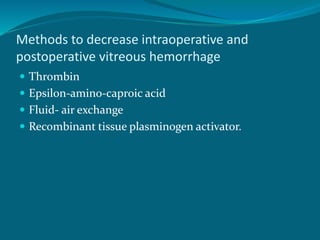
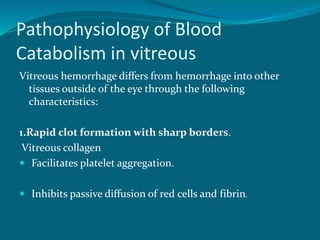
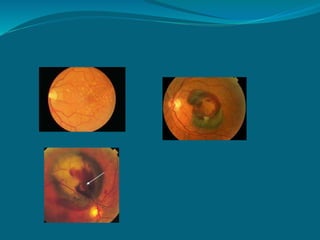
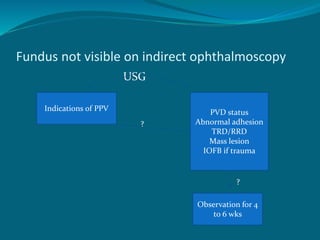
The document discusses vitreous hemorrhage, detailing its definition, pathologic mechanisms, common causes, and various types. It outlines the etiology, prognosis, and management strategies, including observation, laser photocoagulation, and vitrectomy. Additionally, it highlights relevant complications, evaluation methods, and advancements in surgical techniques for treating this condition.