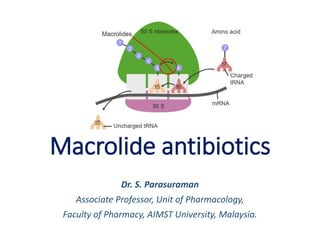
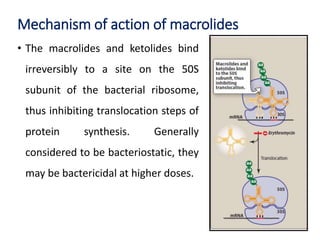
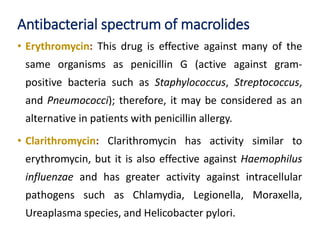
This document discusses macrolide antibiotics, including their structure, examples (erythromycin, azithromycin), mechanism of action, spectrum of activity, resistance, pharmacokinetics, adverse effects, drug interactions, and contraindications. Macrolides bind to the bacterial ribosome and inhibit protein synthesis, generally being bacteriostatic. Their spectrum includes many gram-positive bacteria and some intracellular pathogens. Resistance can occur via efflux pumps or ribosomal mutations. Adverse effects include gastrointestinal issues and ototoxicity. Macrolides can interact with drugs metabolized by CYP450 enzymes.
![Macrolide antibiotics
• The macrolides are a group of antibiotics with a
macrocyclic lactone structure to which one or more deoxy
sugars are attached.
• Erythromycin is the first member discovered in the 1950s,
Roxithromycin, Clarithromycin, Telithromycin and
Azithromycin are the later additions.
• Telithromycin, a semisynthetic derivative of erythromycin,
is the first “ketolide [Ketolides are derived from
erythromycin by substituting the cladinose sugar with a
keto-group]” antimicrobial agent.](https://image.slidesharecdn.com/l10macrolideantibiotics-220504084216/85/Macrolide-antibiotics-pptx-2-320.jpg)


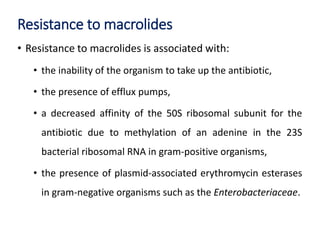


![Reference: Macrolides. Available in https://tmedweb.tulane.edu/pharmwiki/doku.php/macrolides [Last assessed on 24 Apr. 2022]](https://image.slidesharecdn.com/l10macrolideantibiotics-220504084216/85/Macrolide-antibiotics-pptx-13-320.jpg)