This document discusses drugs used to treat amoebiasis, an infection caused by Entamoeba histolytica. It describes the life cycle and stages of E. histolytica, as well as the different types of amoebiasis. The main drugs discussed are metronidazole, tinidazole, emetine, diloxanide furoate, chloroquine, and paromomycin. It provides details on the mechanisms of action, pharmacokinetics, uses, and side effects of these various anti-amoebic drugs.


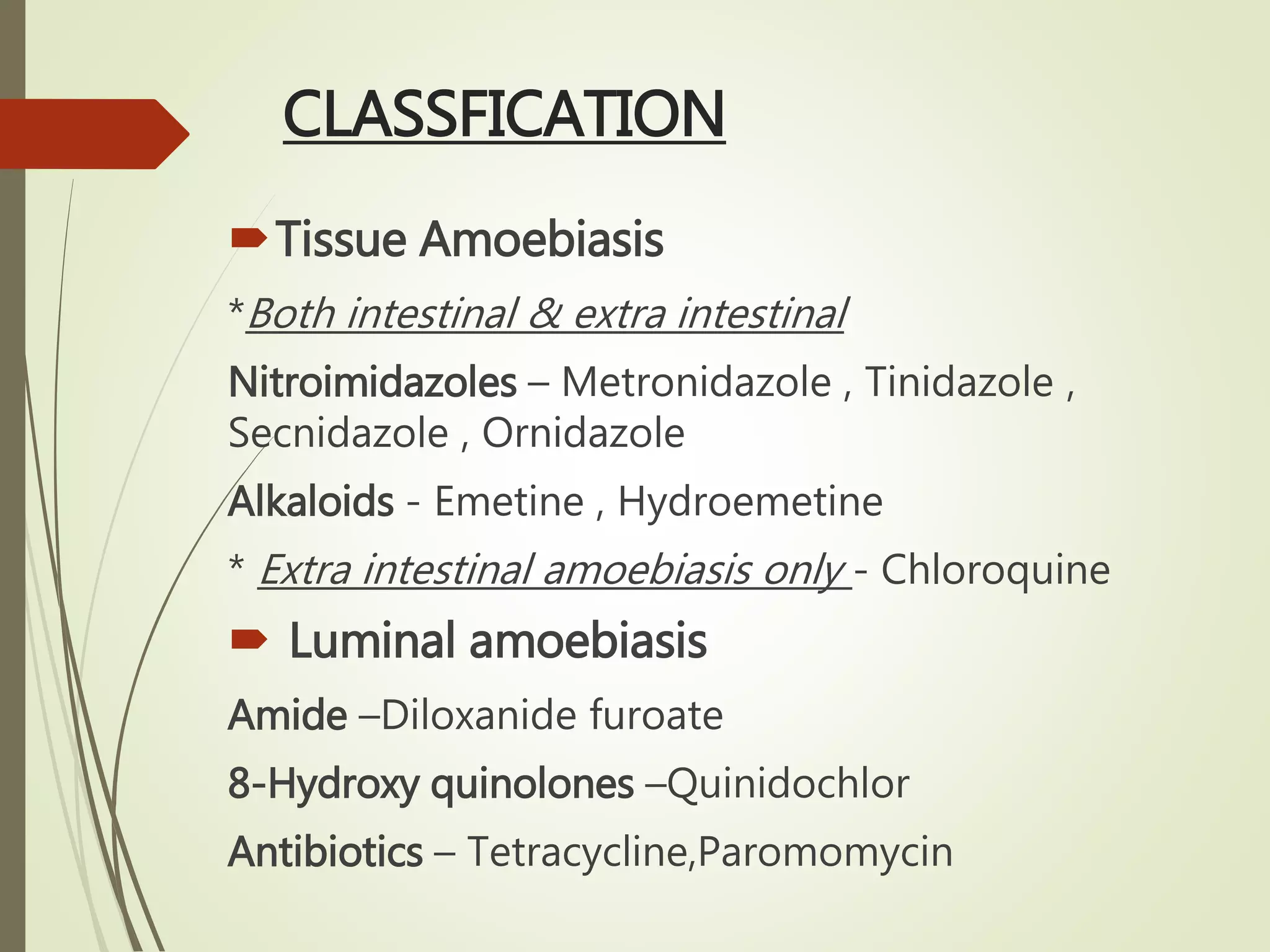






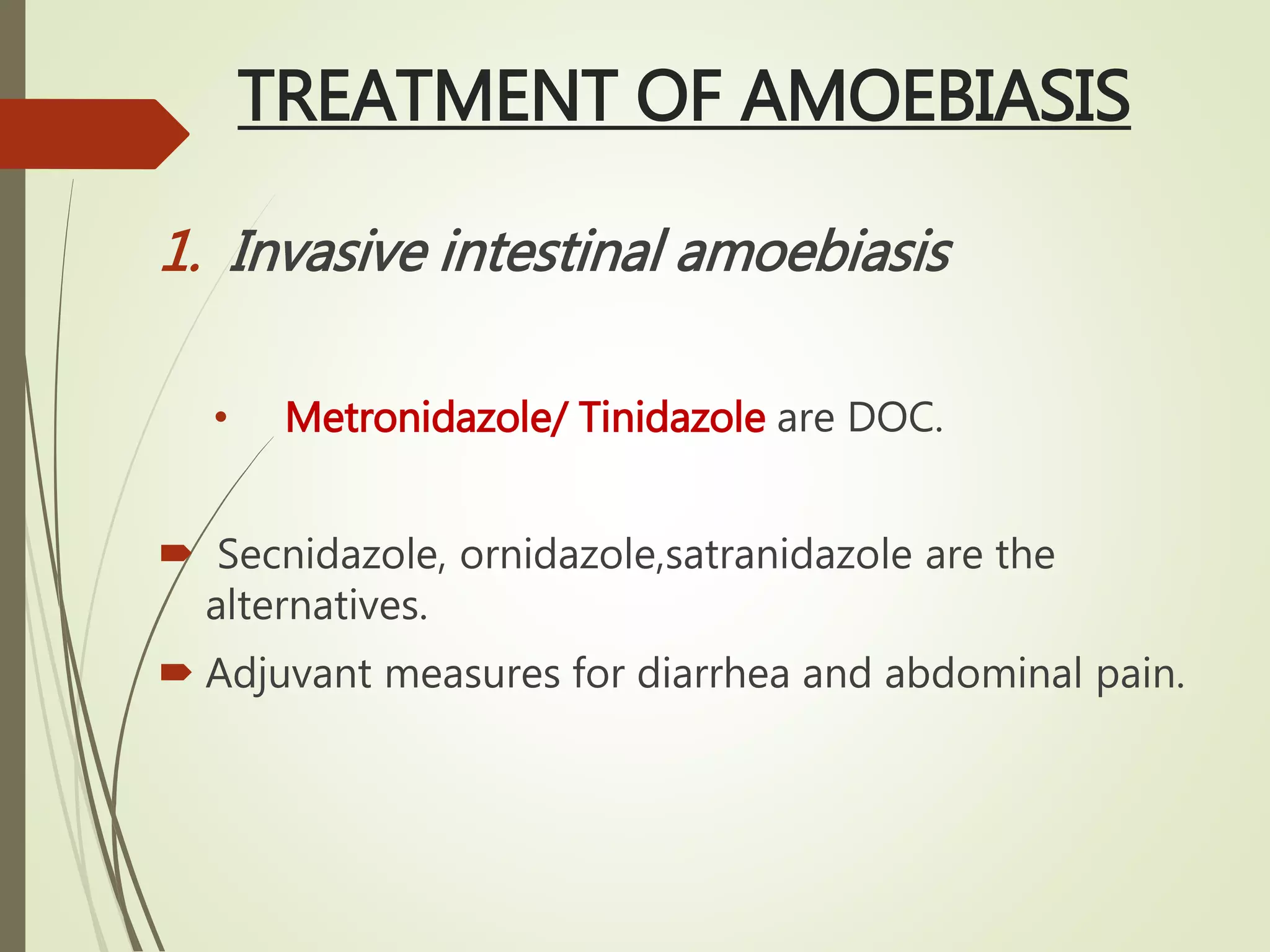
![ Secnidazole : longest t ½ [17-29 hrs]
2 g single dose but for hepatic amoebiasis 1.5 gm
od X5 days
Ornidazole –long t ½ ,similar to Tinidazole
Satranidazole –
better tolerability
No disulfiram reaction
No acetamide metabolite [weak carcinogen]](https://image.slidesharecdn.com/antiprotozoal-copy-160120033604/75/Anti-Amoebic-Drugs-12-2048.jpg)
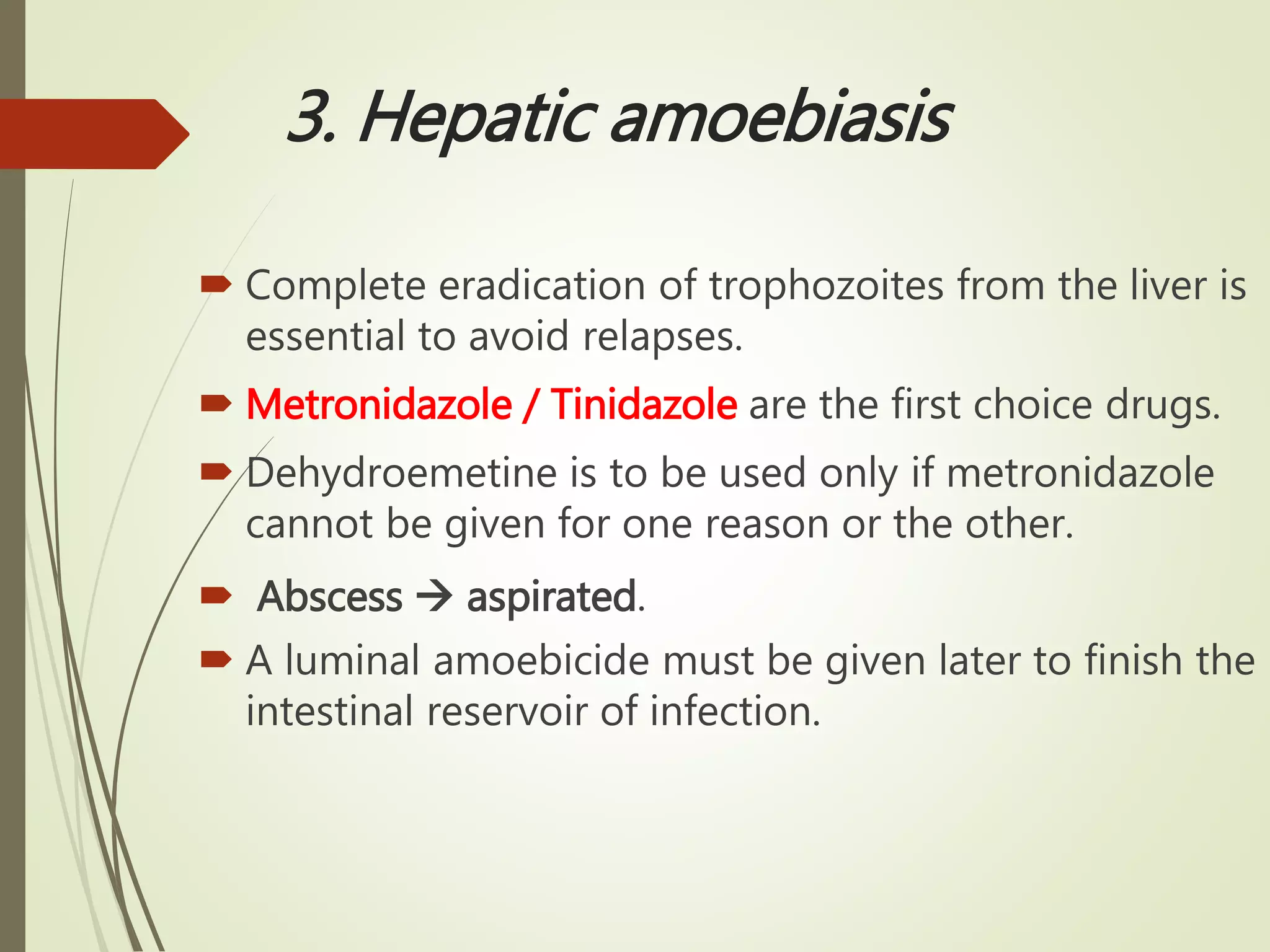
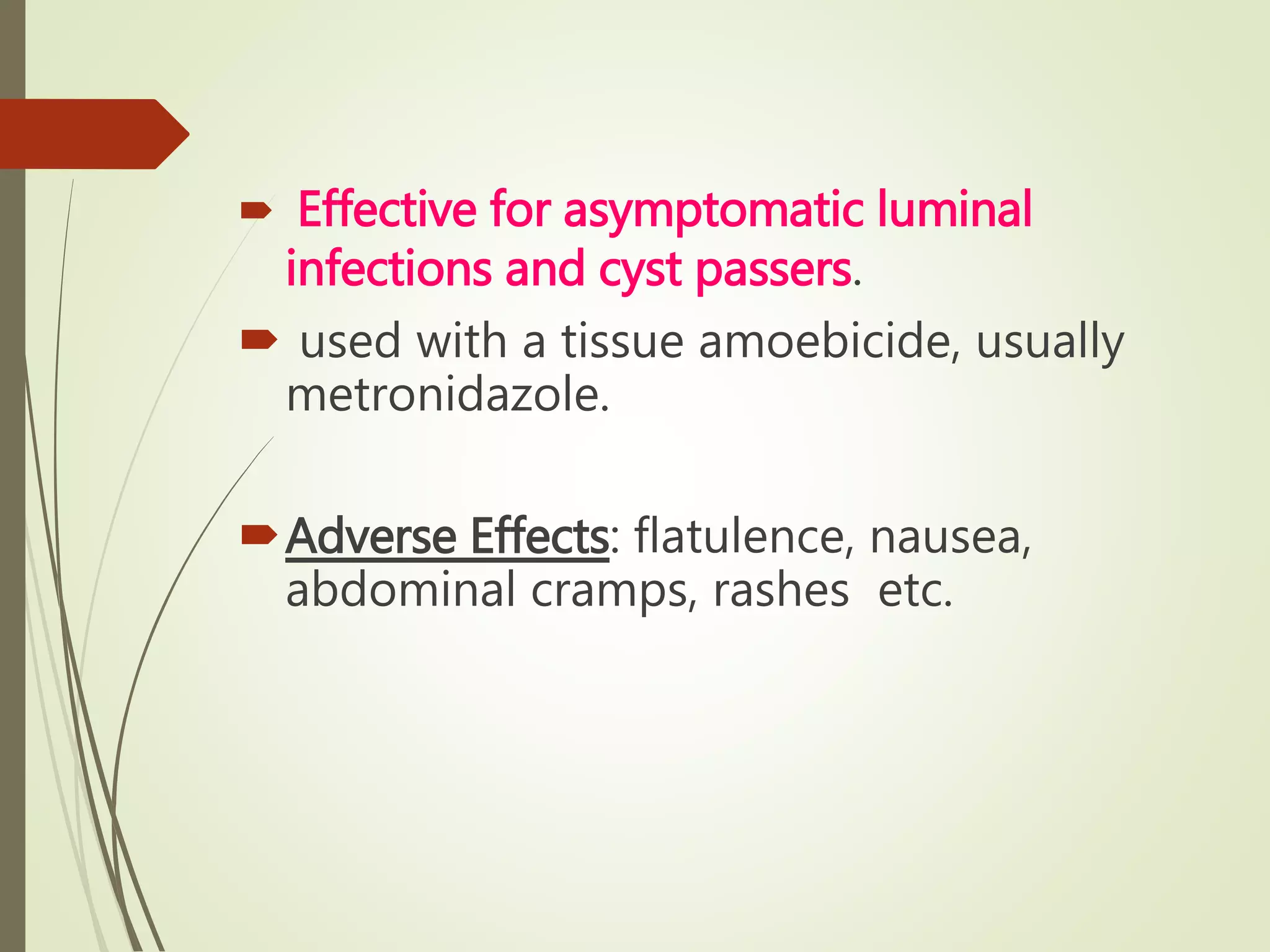
![Emetine and Dehydroemetine
Emetine - alkaloid from Cephaelis ipecacuanha.
Dehydroemetine - a semisynthetic
analog[less cardiotoxic,less cumulative]
are effective against tissue trophozoites of E
histolytica .](https://image.slidesharecdn.com/antiprotozoal-copy-160120033604/75/Anti-Amoebic-Drugs-13-2048.jpg)








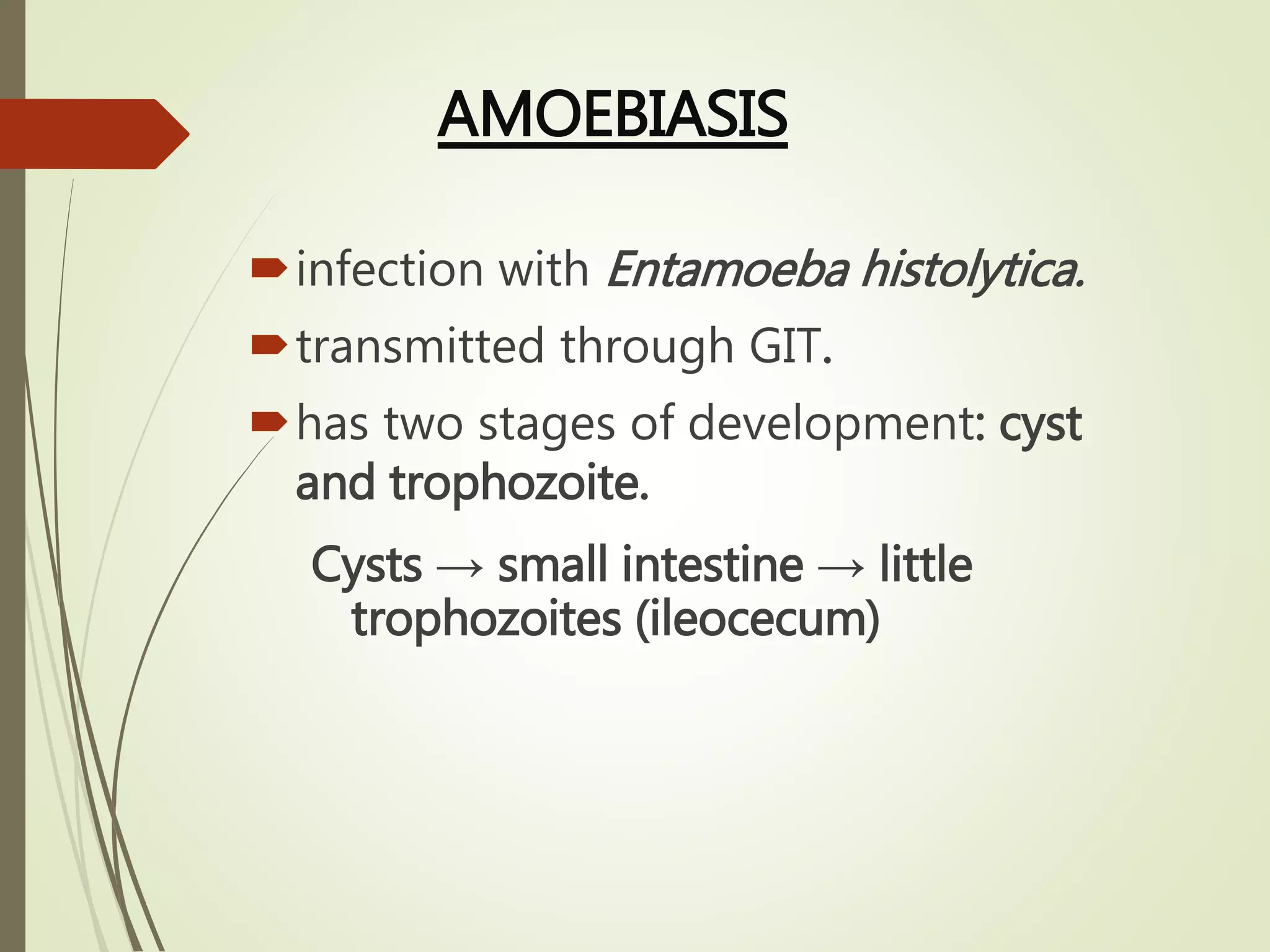
![PK
Prodrug tizoxanide
PFOR inhibitor [essential enzyme p/w of electron
transport metabolism in anaerobic organisms]
Conjugated in liver bile and urine
USE
Amoebic dysentery as luminal amoebicide
Giardiasis, Cryptosporidiosis
ADR
Abd pain, vomiting, head ache…](https://image.slidesharecdn.com/antiprotozoal-copy-160120033604/75/Anti-Amoebic-Drugs-23-2048.jpg)



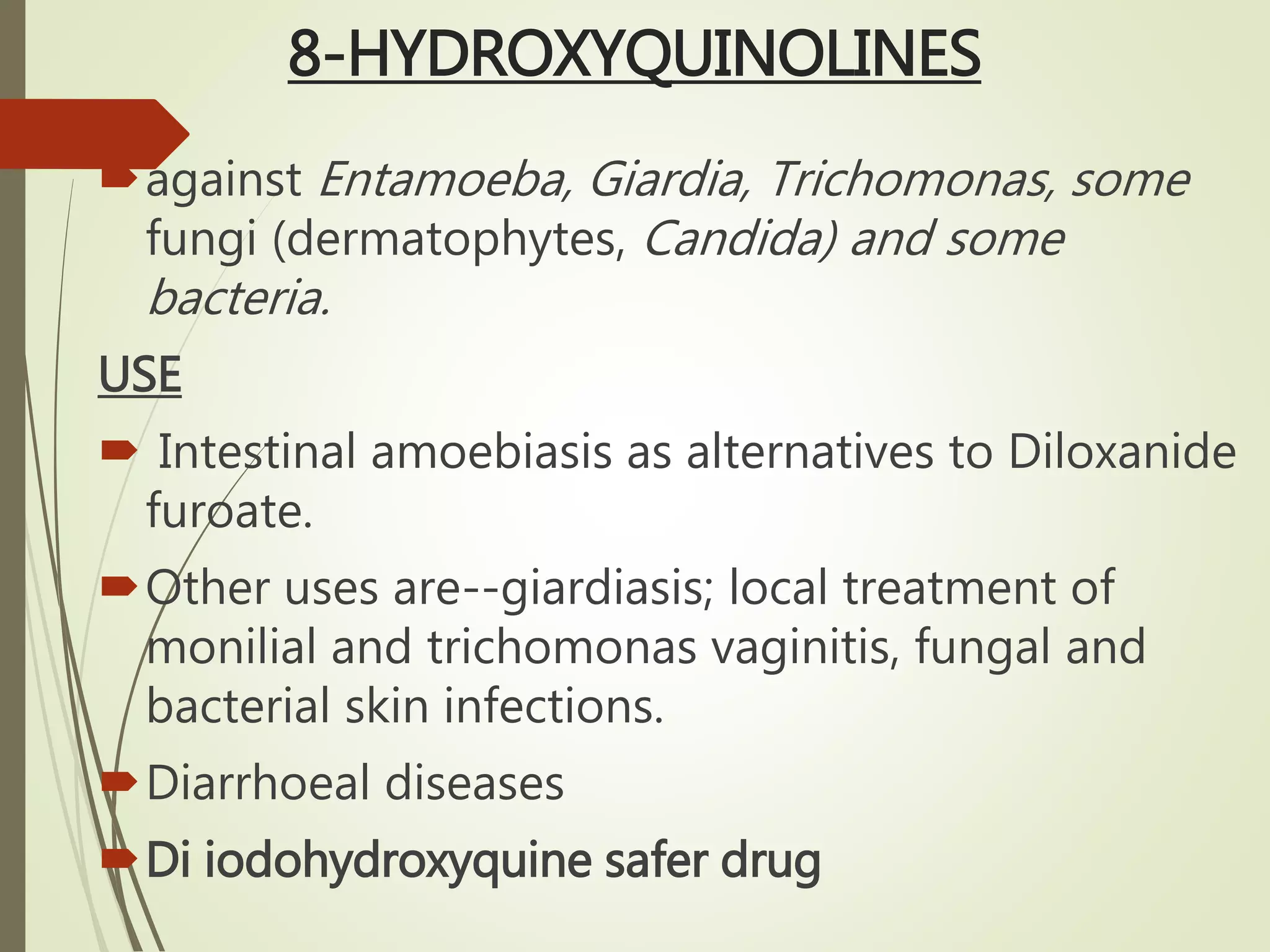
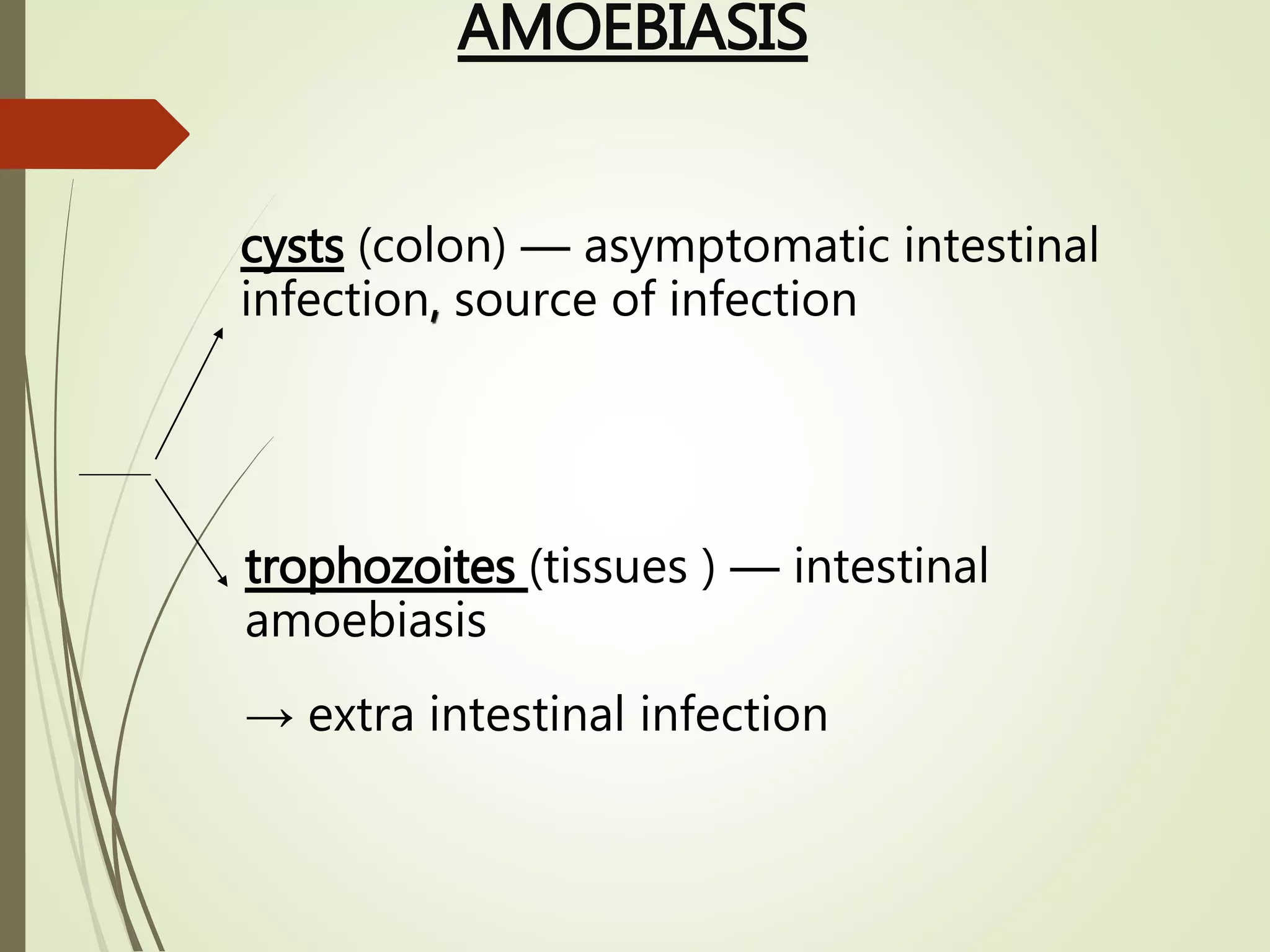
![ ADR
Nausea, transient loose and green stools, pruritus
etc. Goiter prolonged medication.
Iodism (furunculosis, inflammation of mucous
membranes) --due to chronic iodine overload.
Prolonged/repeated use of high doses of
quiniodochlor caused a neuropathic syndrome
called 'subacute myelo-optic neuropathy' (SMON)
India banned only for pediatric patients,
[blindness]. Banned in other countries.](https://image.slidesharecdn.com/antiprotozoal-copy-160120033604/75/Anti-Amoebic-Drugs-28-2048.jpg)