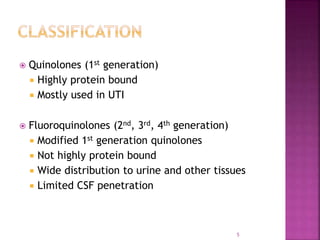
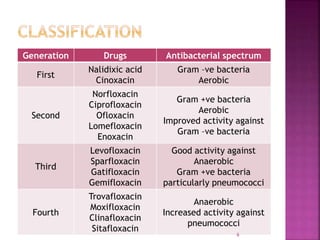
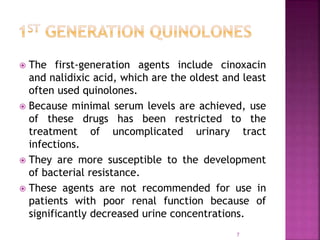
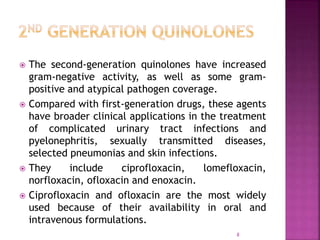
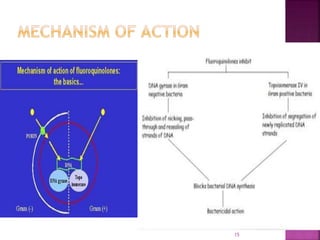
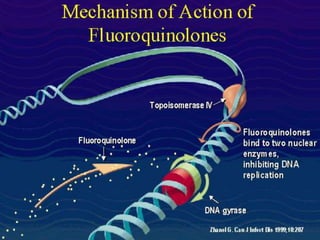
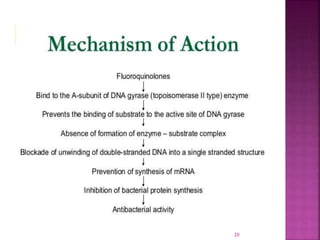
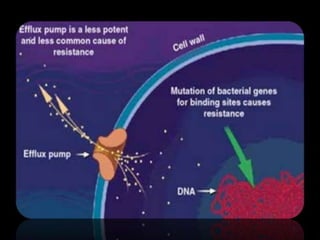
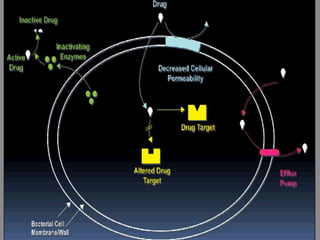
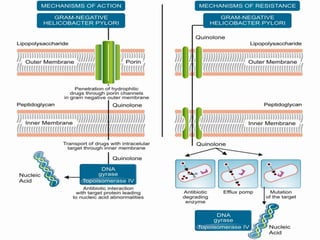
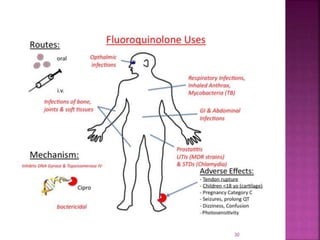
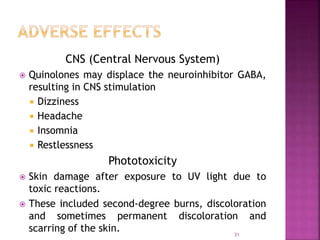
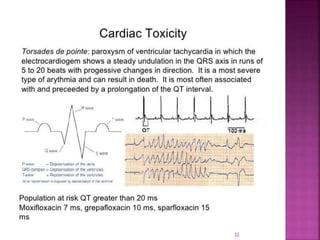
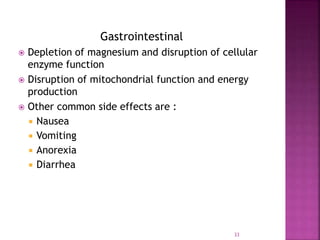
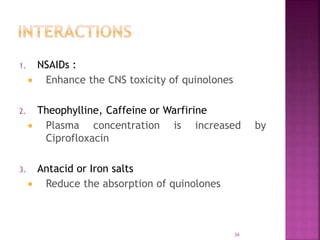
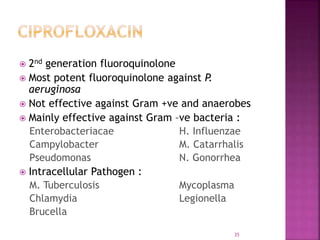
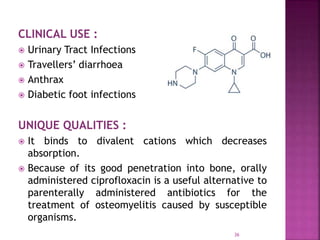
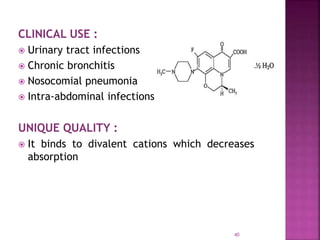
This document provides an overview of quinolones, including their history, classification, mechanisms of action, resistance, pharmacokinetics, uses, adverse effects and interactions. It discusses the four generations of quinolones and specific drugs within each generation. The first generation includes nalidixic acid and is used primarily for UTIs. Later generations have expanded gram positive and atypical pathogen coverage. Common uses include RTIs, UTIs, gastrointestinal and skin infections. Adverse effects include CNS effects, phototoxicity and gastrointestinal issues. Quinolones can interact with NSAIDs, theophylline and antacids. Ciprofloxacin and levofloxacin are discussed in more depth.