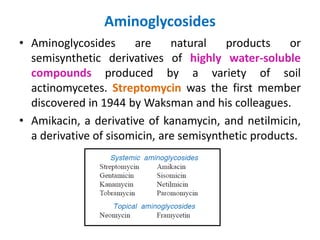
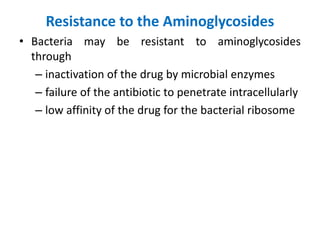
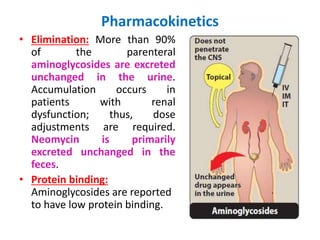
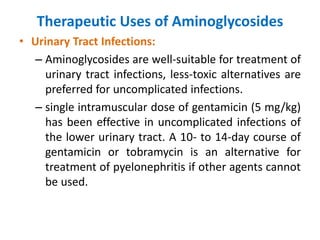
Aminoglycosides are a class of antibiotics that are produced by soil bacteria. They are primarily used to treat infections caused by aerobic gram-negative bacteria and some are used for mycobacterial infections. Aminoglycosides work by binding to bacterial ribosomes which interferes with protein synthesis. They have concentration-dependent bactericidal activity against many gram-negative organisms but limited activity against gram-positive bacteria. Common adverse effects include ototoxicity and nephrotoxicity. Therapeutic drug monitoring is important when using aminoglycosides to minimize toxicity risks.