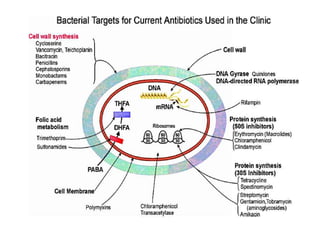
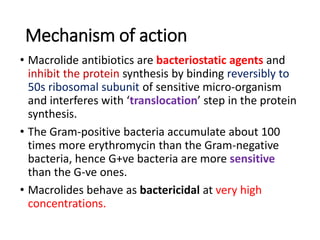
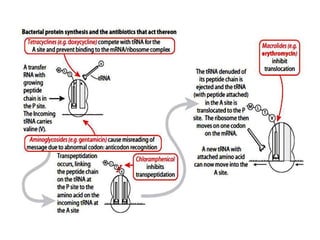
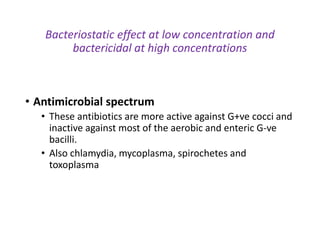
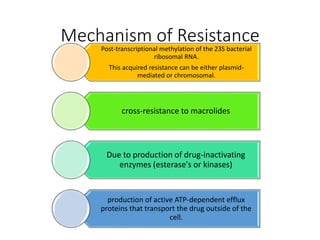
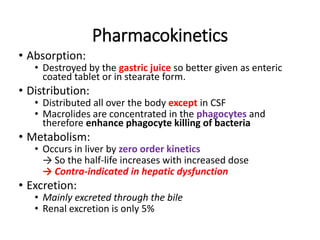
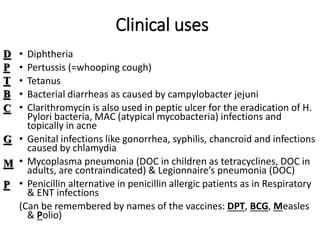
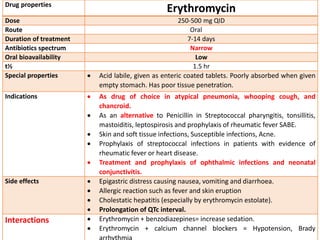
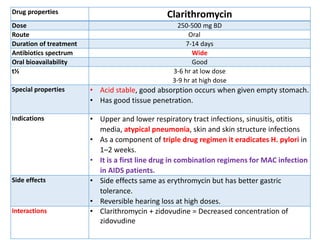
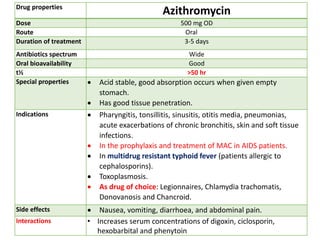
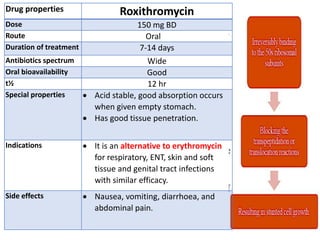
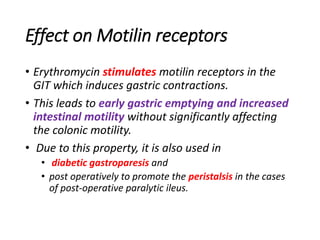
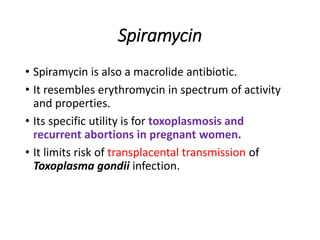
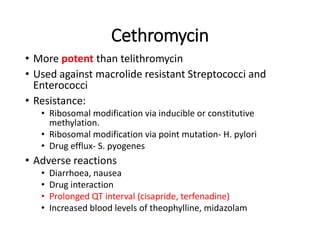
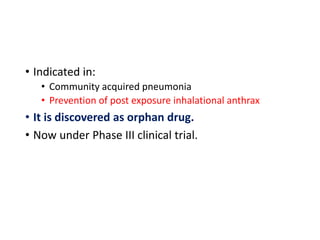
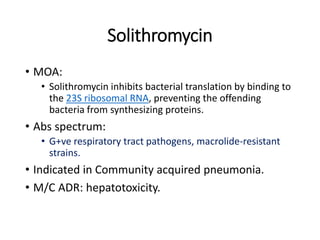
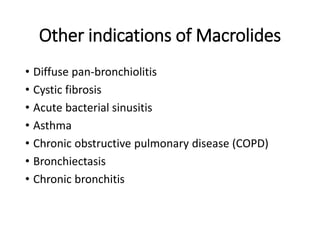
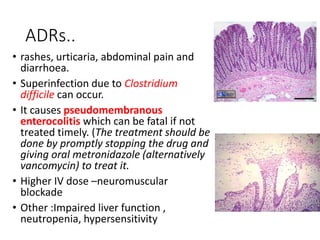
This document discusses macrolide antibiotics, including their mechanism of action, types, and uses. It describes several macrolide antibiotics like erythromycin, clarithromycin, azithromycin, and roxithromycin. It covers their mechanisms of action, spectra of activity, pharmacokinetics, clinical uses, side effects, and interactions. It also briefly discusses newer macrolides like telithromycin and ketolides, as well as the lincosamide antibiotic clindomycin.