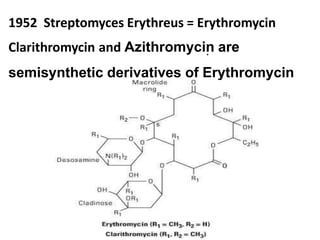
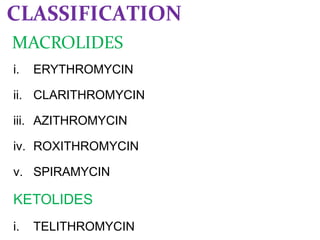
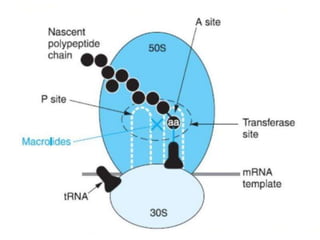
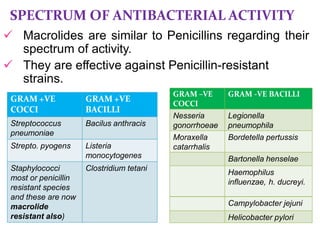
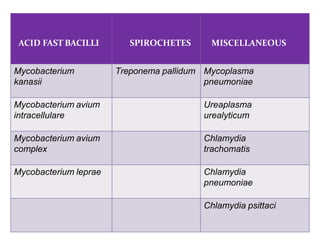
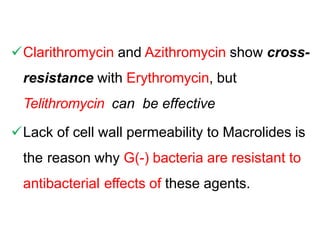
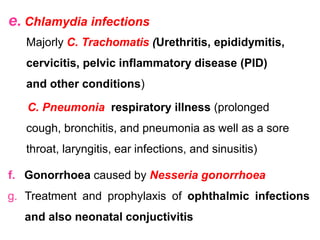
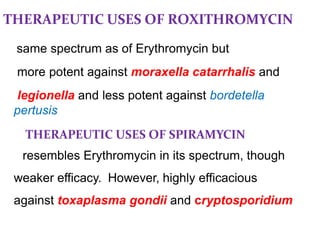
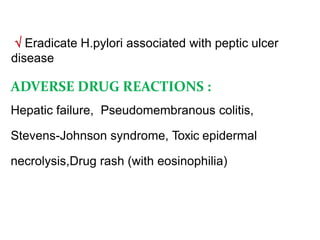
Macrolides are a class of antibiotics characterized by a macrocyclic lactone ring with attached sugars. Erythromycin was the first macrolide discovered from the bacterium Streptomyces erythreus in 1952. It inhibits bacterial protein synthesis by binding the 50S ribosomal subunit. Macrolides are effective against many gram-positive bacteria and some gram-negatives. Common macrolides include erythromycin, clarithromycin, azithromycin, and roxithromycin. They are used to treat respiratory, skin, and sexually transmitted infections. Adverse effects include gastrointestinal issues and potentially serious reactions like prolonged QT interval.