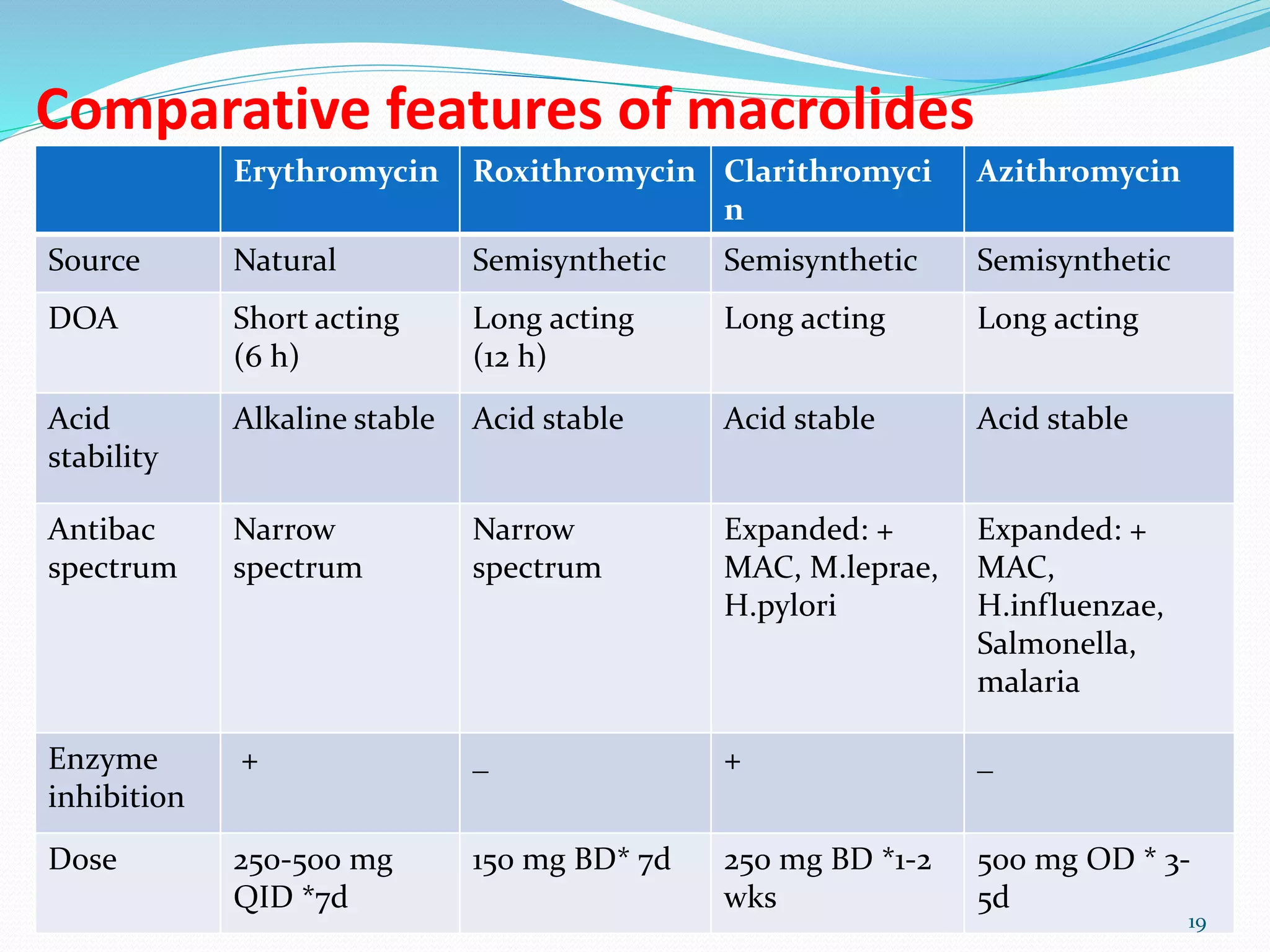
This document discusses macrolide antibiotics, including erythromycin, roxithromycin, azithromycin, and clarithromycin. It provides details on their origins, mechanisms of action, antimicrobial spectra, pharmacokinetics, uses, and adverse effects. The key points are:
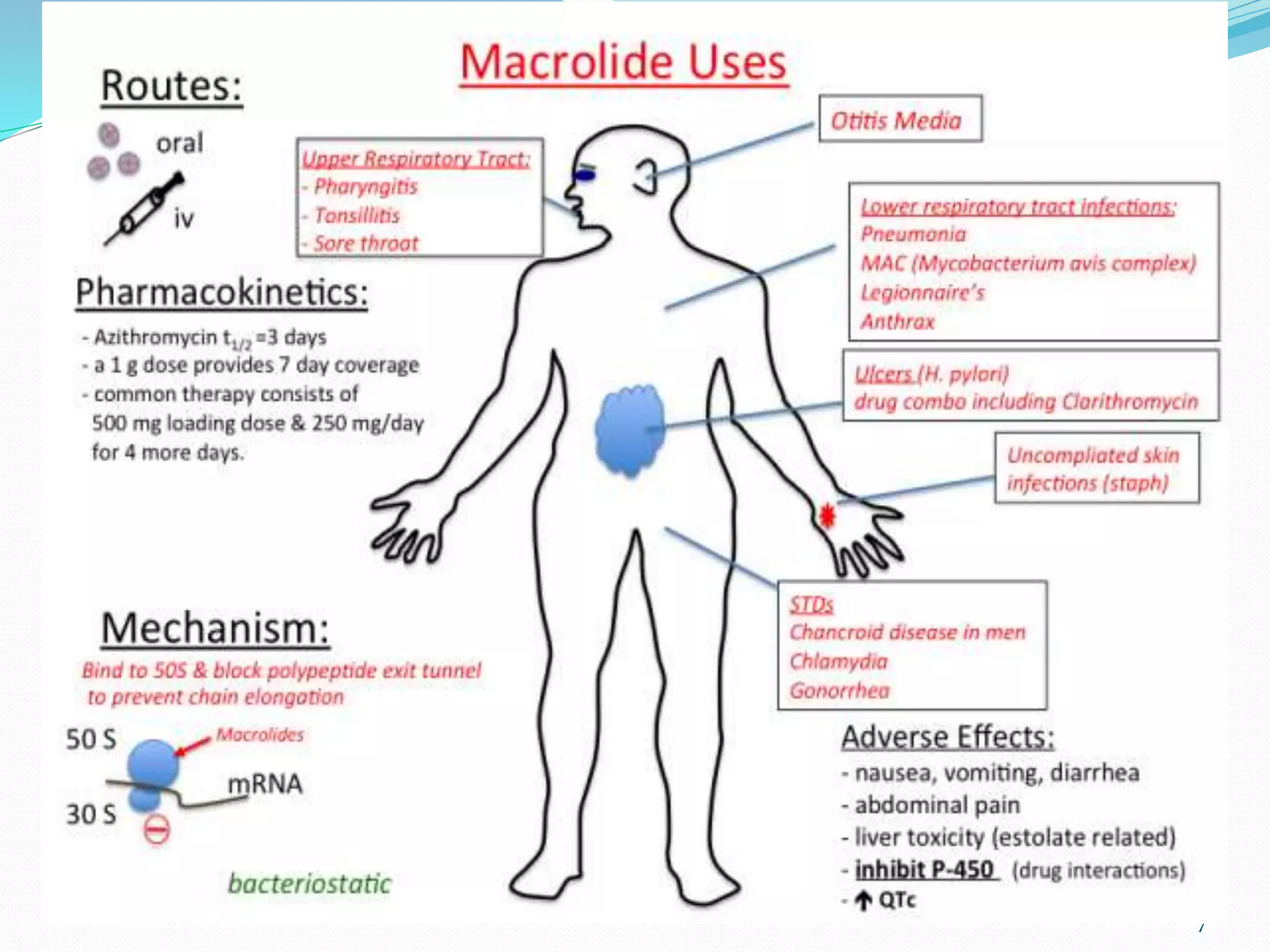
- Macrolides are a class of antibiotics derived from the bacterium Streptomyces that inhibit bacterial protein synthesis.
- They are mainly effective against gram-positive bacteria and some gram-negatives.
- They bind to the 50S ribosomal subunit to prevent bacterial protein synthesis.
- Newer macrolides like azithromycin have expanded spectra and more favorable dosing compared to eryth