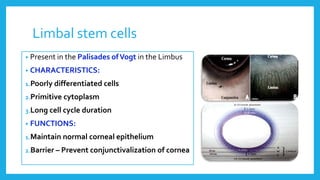
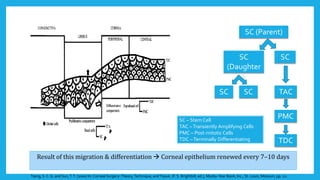
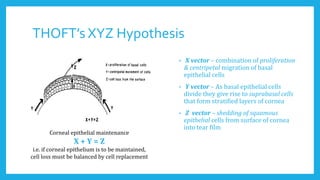
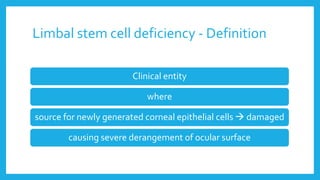
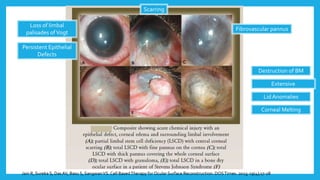
1) Limbal stem cells are located in the palisades of Vogt region of the limbus and are responsible for maintaining the normal corneal epithelium. Limbal stem cell deficiency occurs when the source of these cells is damaged, causing severe problems to the ocular surface.
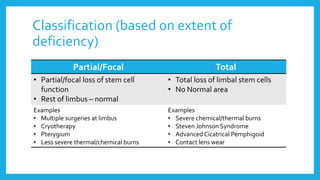
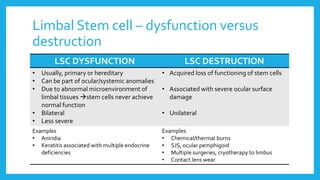
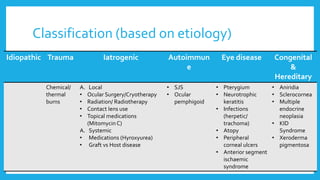
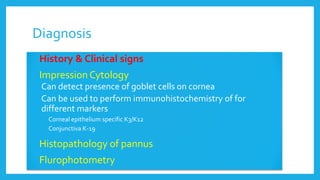
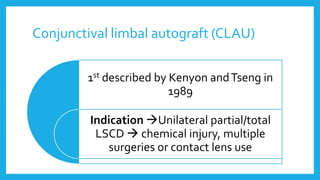
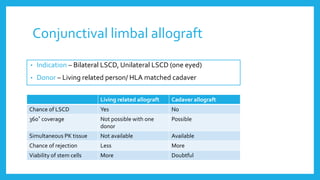
2) Limbal stem cell deficiency can be partial or total, and is classified based on extent and etiology. Common causes include chemical/thermal burns, Stevens-Johnson syndrome, and multiple ocular surgeries.
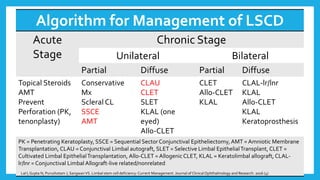
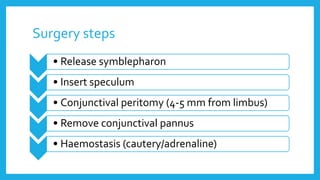
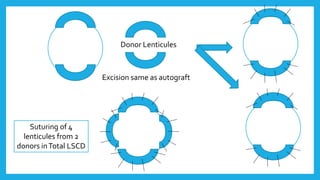
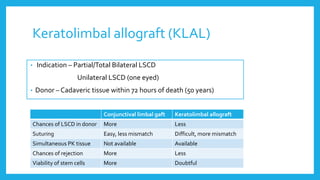
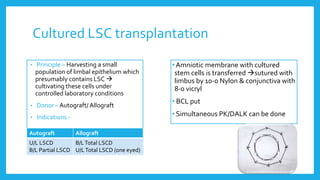
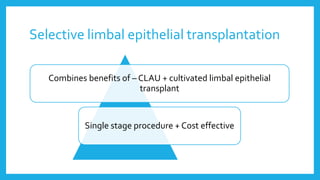
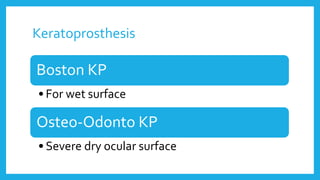
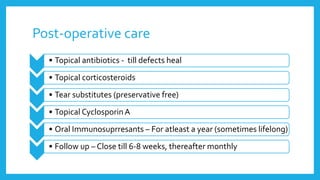
3) Management is based on the extent and severity of deficiency, and involves steps from conservative treatment to more invasive procedures like limbal stem cell transplantation or keratoprosthesis. The goal is to replace