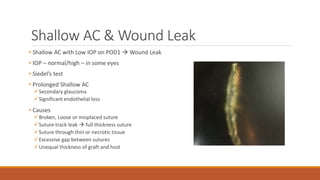
This document discusses various complications that can occur after keratoplasty (corneal transplantation). It summarizes early post-operative complications such as shallow anterior chamber, wound leak, iris incarceration, wound dehiscence, and suture-related problems. It also discusses late complications that can occur months or years after surgery, including graft rejection, infectious crystalline keratopathy, corneal membranes, cataract, astigmatism, glaucoma, and recurrence of the original recipient corneal disorder. For each complication, the document provides details on causes, risk factors, clinical features, prevention strategies and management approaches.