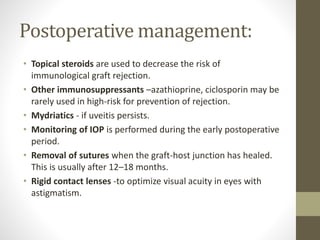
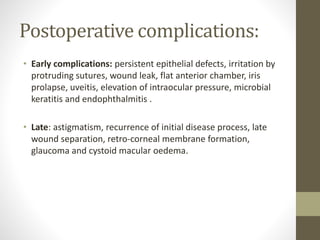
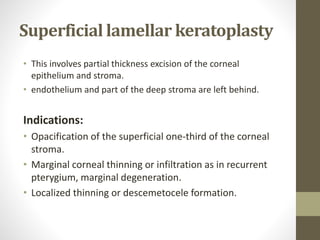
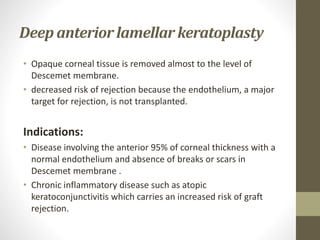
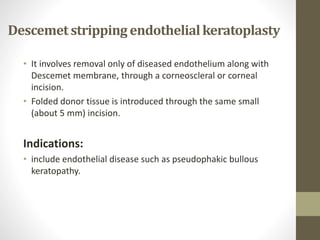
This document discusses different types of keratoplasty procedures including penetrating keratoplasty, lamellar keratoplasty, and Descemet stripping endothelial keratoplasty. Penetrating keratoplasty involves replacing the entire diseased cornea and is used for conditions involving all corneal layers. Lamellar keratoplasty replaces only partial layers of the cornea. Deep anterior lamellar keratoplasty removes tissue to the level of Descemet's membrane while Descemet stripping endothelial keratoplasty only replaces the diseased endothelium and Descemet's membrane through a small incision.