This document summarizes various types of corneal dystrophies:
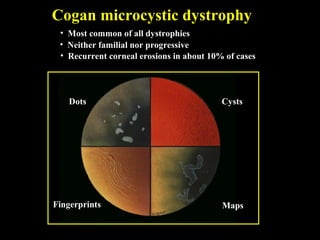
- Anterior corneal dystrophies include Cogan microcystic, Reis-Bucklers, Meesmann, and Schnyder dystrophies.
- Stromal dystrophies include lattice types I-III and granular types I-III (Avellino).
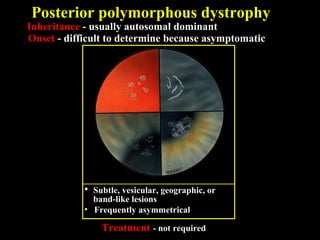
- Posterior dystrophies include Fuchs endothelial and posterior polymorphous dystrophies. Each dystrophy is described in terms of inheritance, onset, symptoms, signs, treatment or progression.