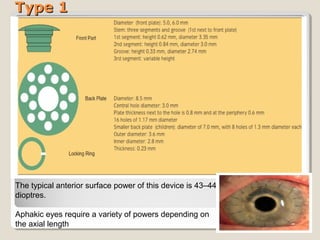
Keratoprosthesis is a surgical procedure where an artificial cornea replaces a severely damaged or diseased natural cornea. It involves implanting an artificial optical cylinder made of clear plastic materials inside the eye with a supporting flange or skirt outside the eye. The Boston KPro is the most commonly used keratoprosthesis device and comes in Type 1 and Type 2 models for different clinical situations. The Osteo-Odonto KPro is a more complex multi-stage procedure that uses the patient's own tooth and surrounding bone to support an artificial cornea for patients with severe dry eye conditions. Keratoprosthesis surgery aims to restore sight for patients with corneal blindness when traditional corneal transplant is not possible or