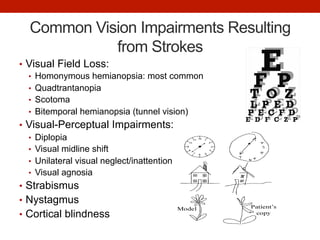
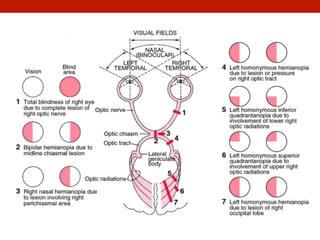
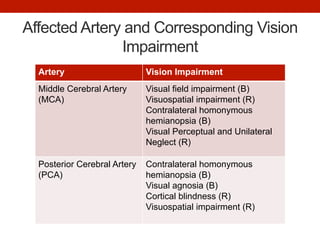
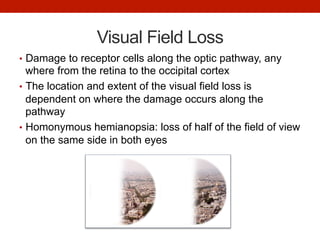
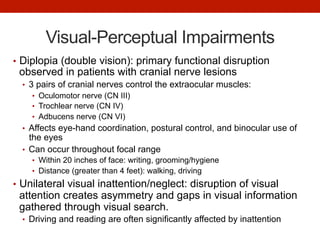
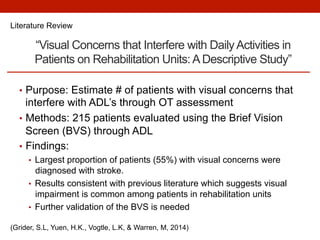
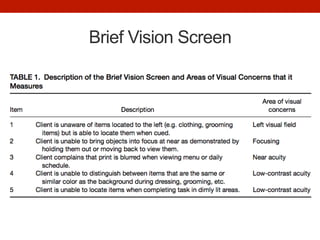
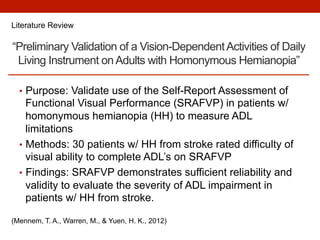
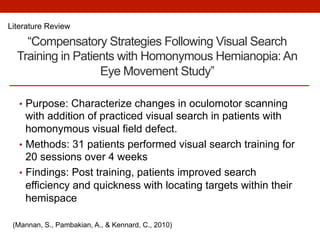
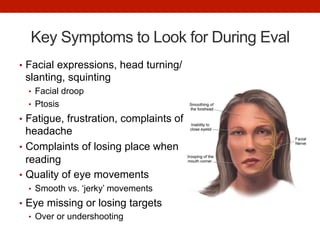
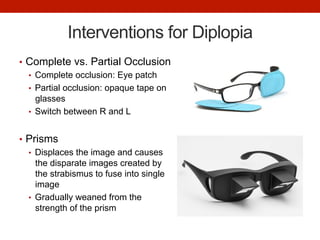
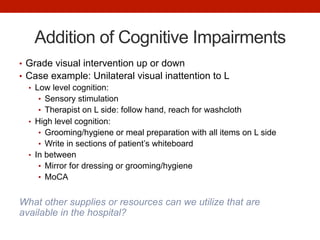
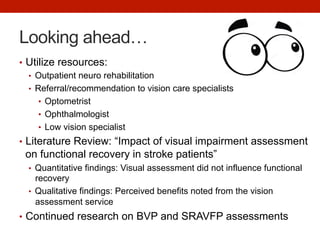
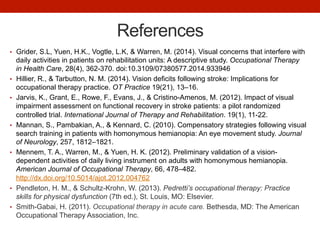
This document discusses vision deficits that can occur after a stroke and how occupational therapists can incorporate vision screening and interventions into inpatient rehabilitation. Approximately 55% of patients in rehabilitation have strokes, which can cause visual field loss, visual perceptual impairments like diplopia or neglect, and other issues. Assessments like the Brief Vision Screen can identify patients' visual concerns. Interventions may include visual scanning exercises, use of prisms or occlusion for diplopia, positioning items on the affected side, and adapting the level of support based on cognition. Continued research is needed on assessment tools and addressing vision can benefit patients' functional recovery.