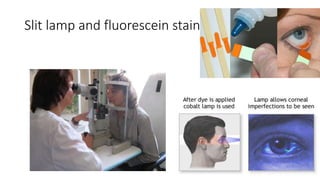
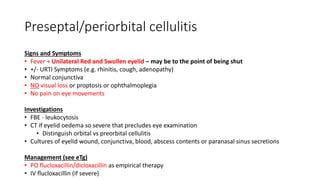
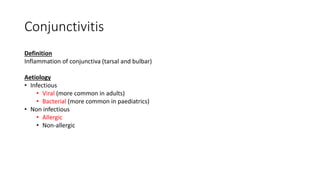
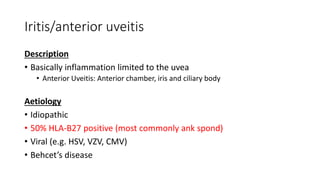
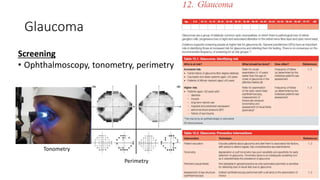
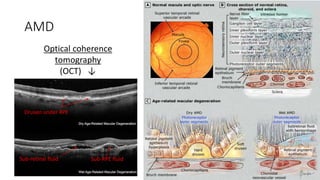
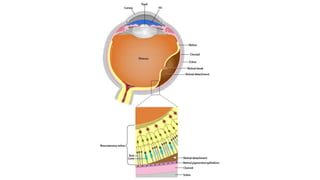
This document summarizes an ophthalmology lecture covering general eye anatomy, history taking, examination techniques, and differentials for common ophthalmic presentations like red eye, acute vision loss, and floaters. Key topics discussed include anatomy of the eye and blood supply, general ophthalmic history and exam including visual acuity testing and slit lamp use, differentials for red eye by level of acuity and pain, management of foreign bodies and chemical injuries, and differences between preseptal and orbital cellulitis. Common conditions like conjunctivitis are also reviewed in terms of etiology, signs, and treatment.