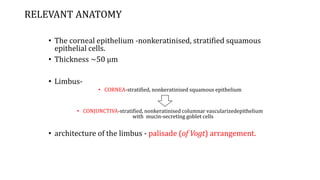
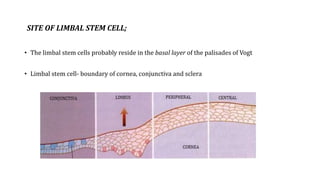
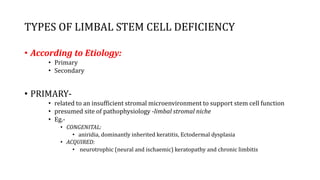
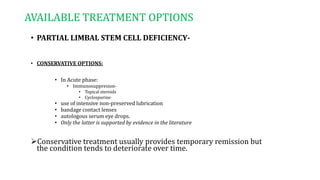
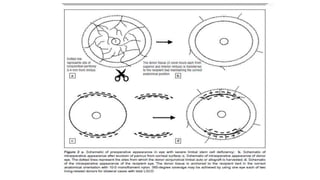
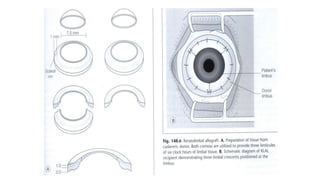
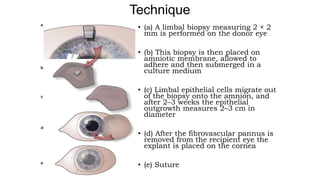
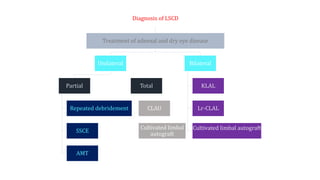
Limbal stem cell deficiency can be caused by various factors and presents with conjunctivalization of the cornea. Diagnosis involves identifying conjunctival goblet cells on the cornea through impression cytology or immunohistochemistry. Treatment depends on the severity and extent of involvement. For partial involvement, conservative options include medications and debridement while more severe cases require ocular surface reconstruction through limbal stem cell transplantation techniques like conjunctival limbal autograft. Emerging treatments involve ex vivo expansion of limbal stem cells to minimize donor tissue requirements.