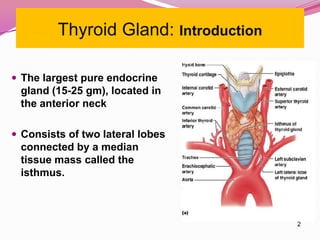
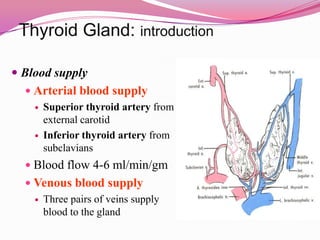
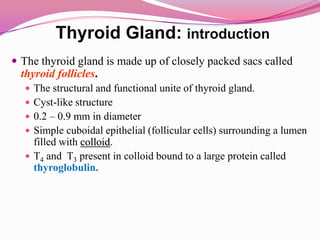
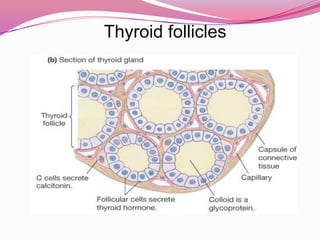
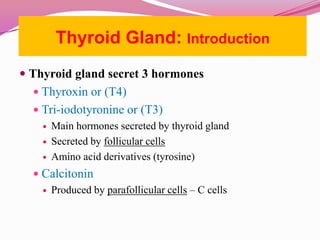
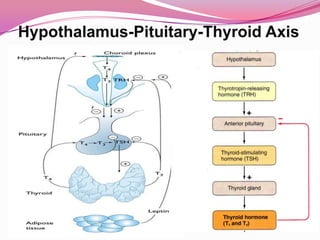
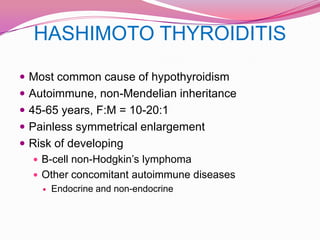
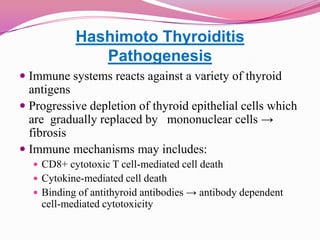
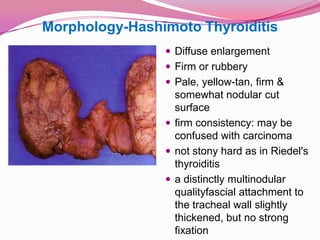
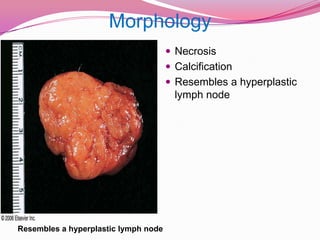
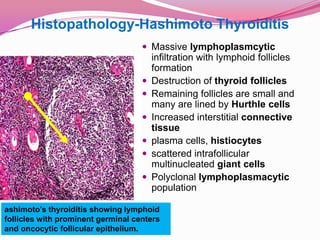
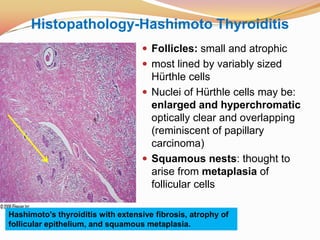
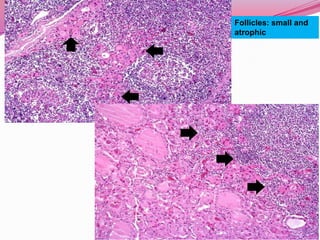
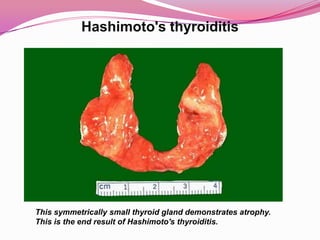
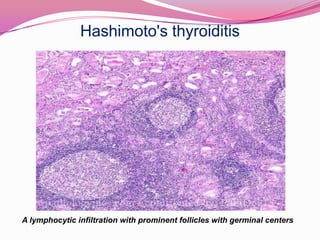
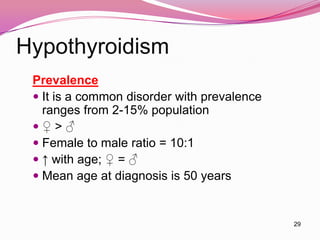
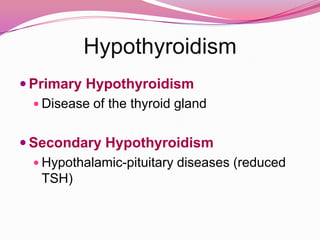
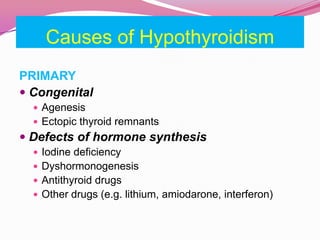
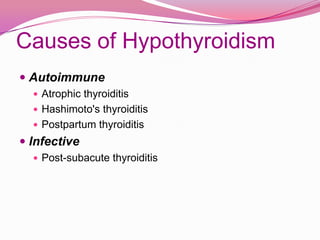
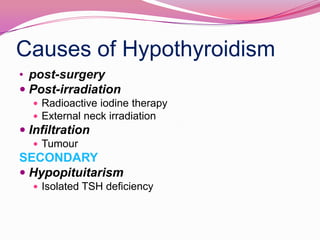
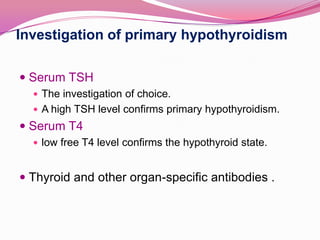
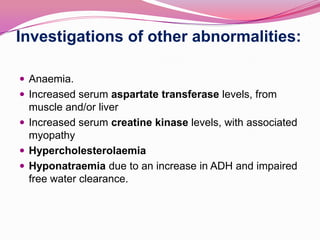
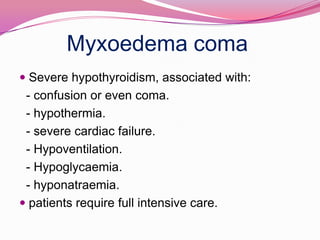
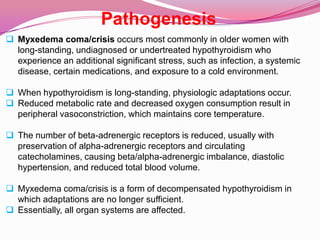
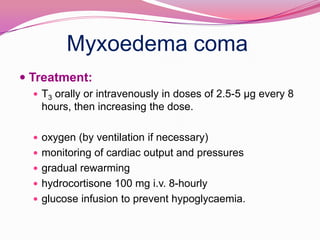
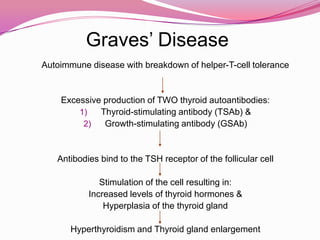
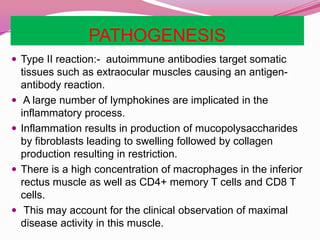
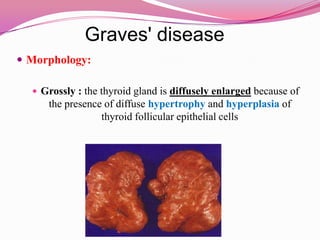
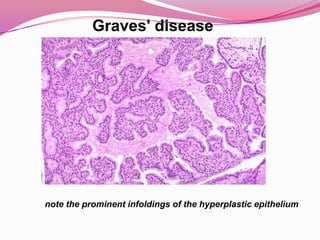
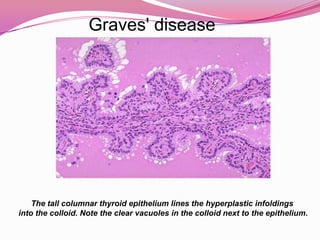
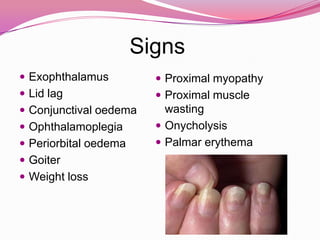
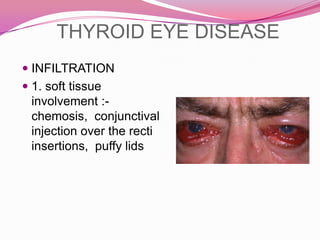
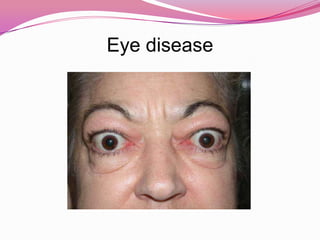
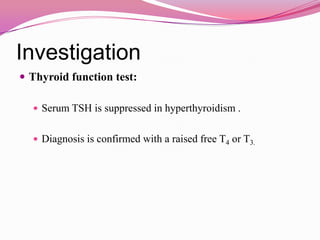
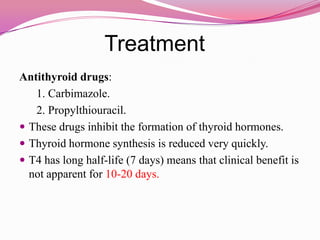
The document provides information about thyroid gland disorders including hypothyroidism and hyperthyroidism. It discusses the anatomy and blood supply of the thyroid gland. It describes Hashimoto's thyroiditis as the most common cause of hypothyroidism due to an autoimmune reaction. Graves' disease is outlined as the most common cause of hyperthyroidism, also caused by an autoimmune process involving thyroid stimulating antibodies. The clinical features, investigations, and treatment approaches for hypothyroidism and hyperthyroidism are summarized.