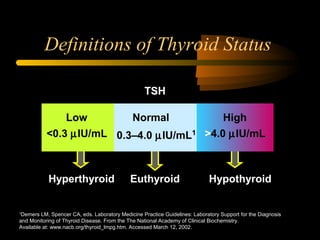
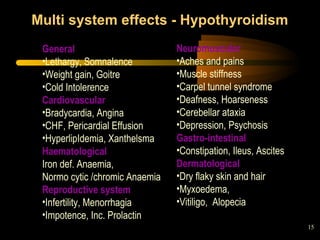
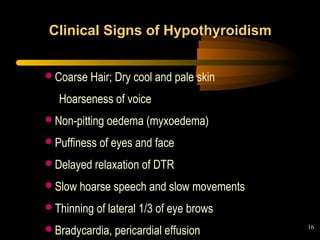
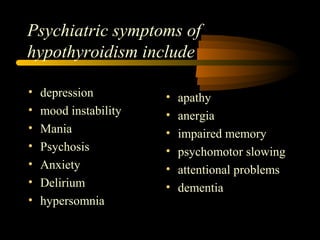
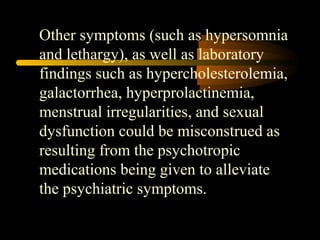
1. Thyroid dysfunction can cause a variety of psychiatric manifestations including depression, mood instability, psychosis, anxiety, and impaired memory. Hypothyroidism in particular can mimic symptoms of mental illnesses.
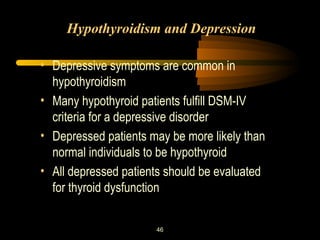
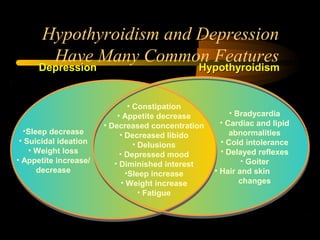
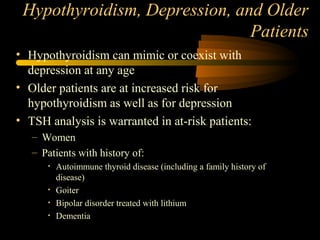
2. Depression is a common symptom of hypothyroidism, and depressed patients may be more likely to have underlying thyroid problems. Treating thyroid dysfunction is important for alleviating associated psychiatric symptoms.
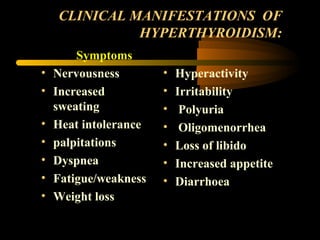
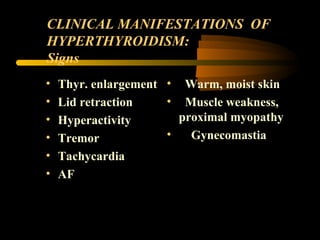
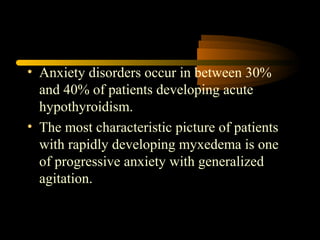
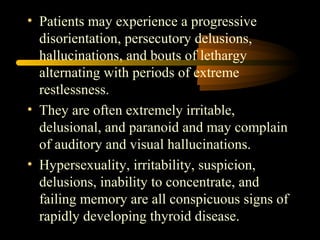
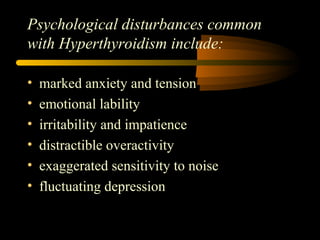
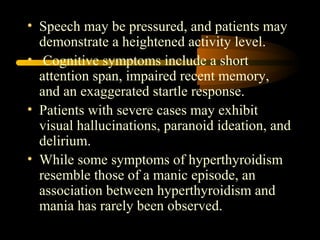
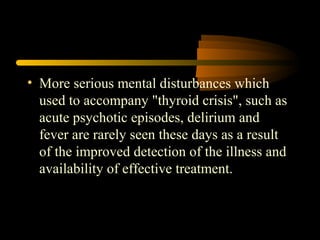
3. Hyperthyroidism can also cause psychiatric issues in a significant percentage of patients, with anxiety being very common. Between 1-20% of hyperthyroid patients experience psychosis.