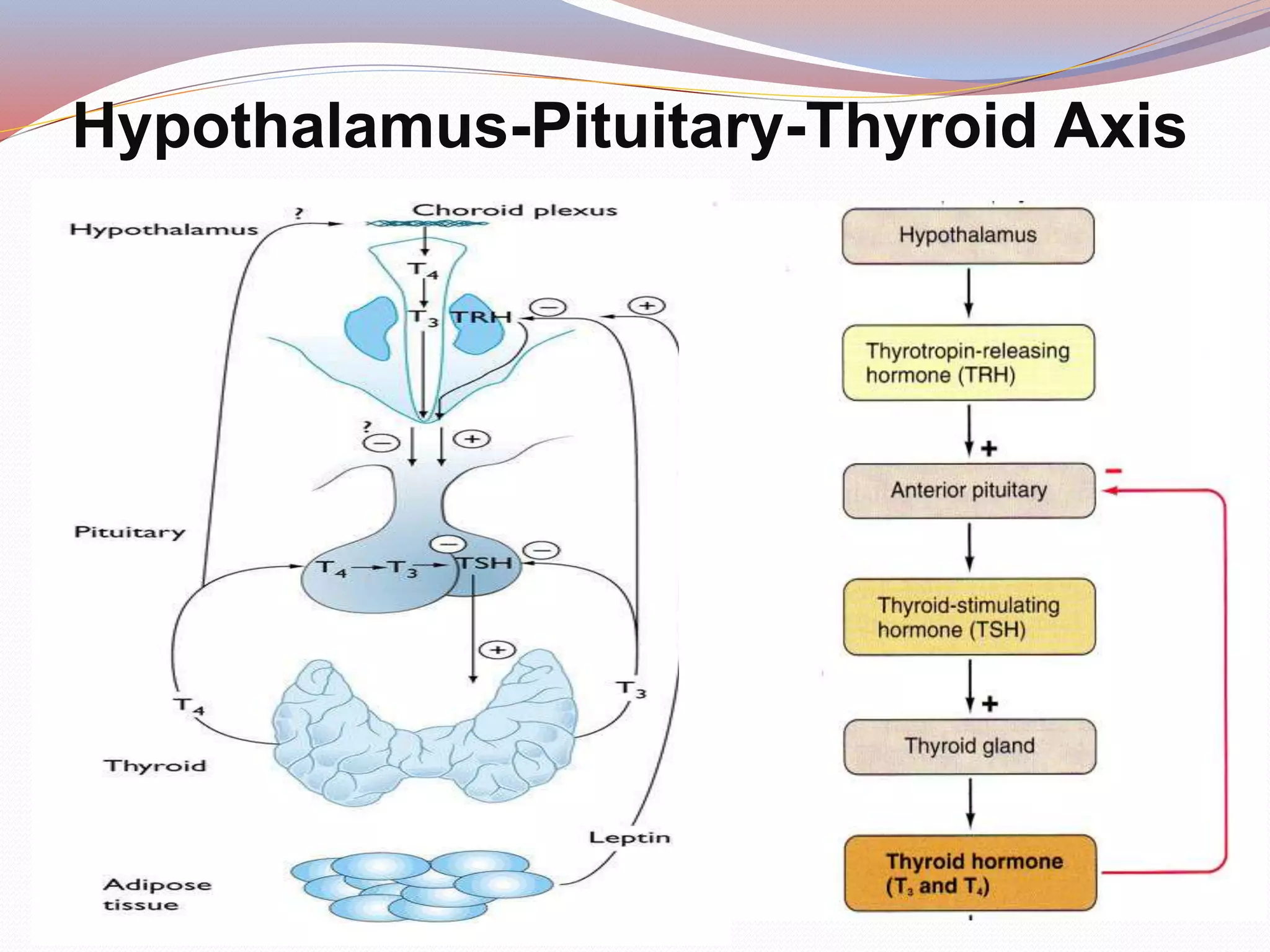
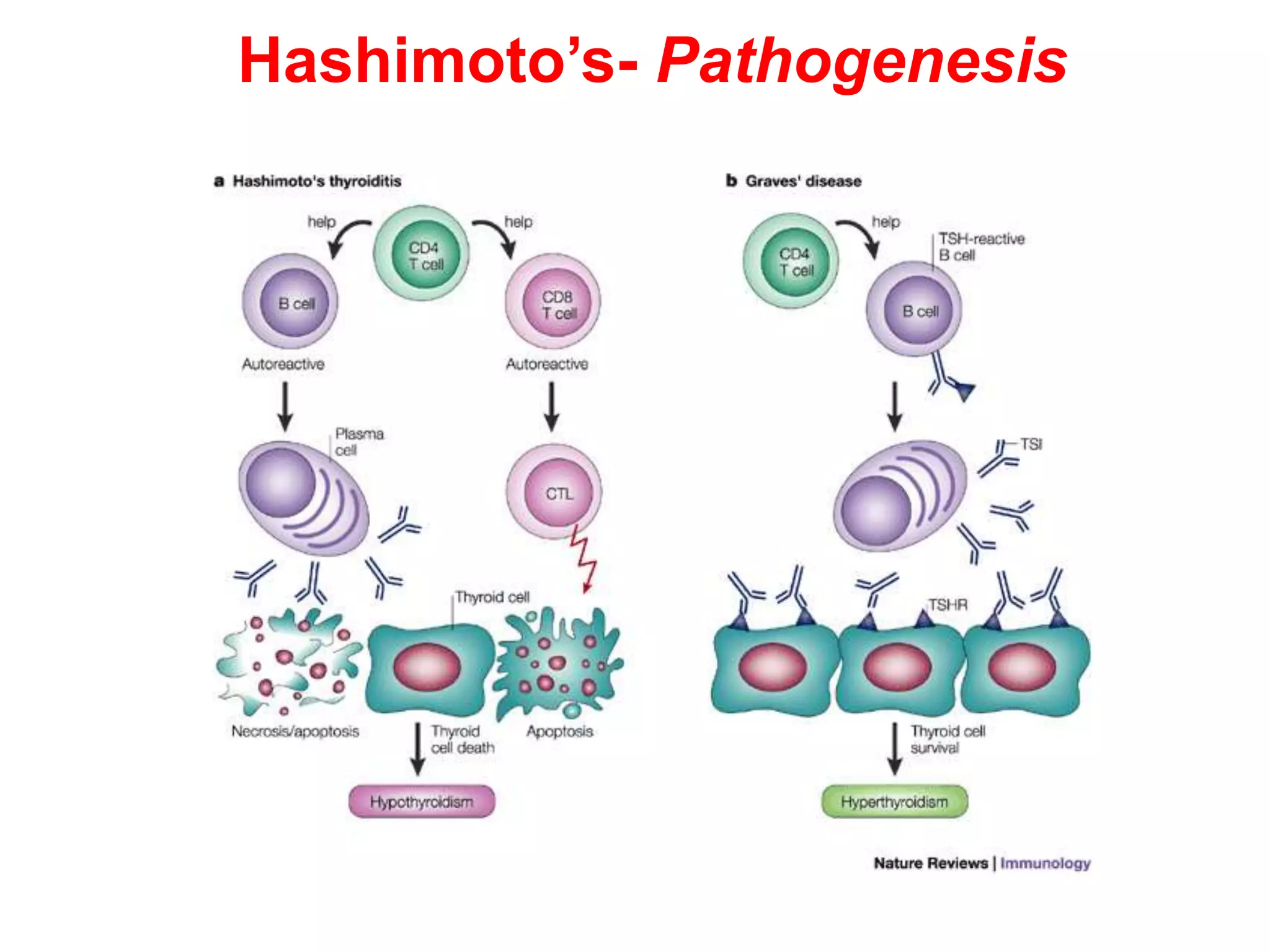
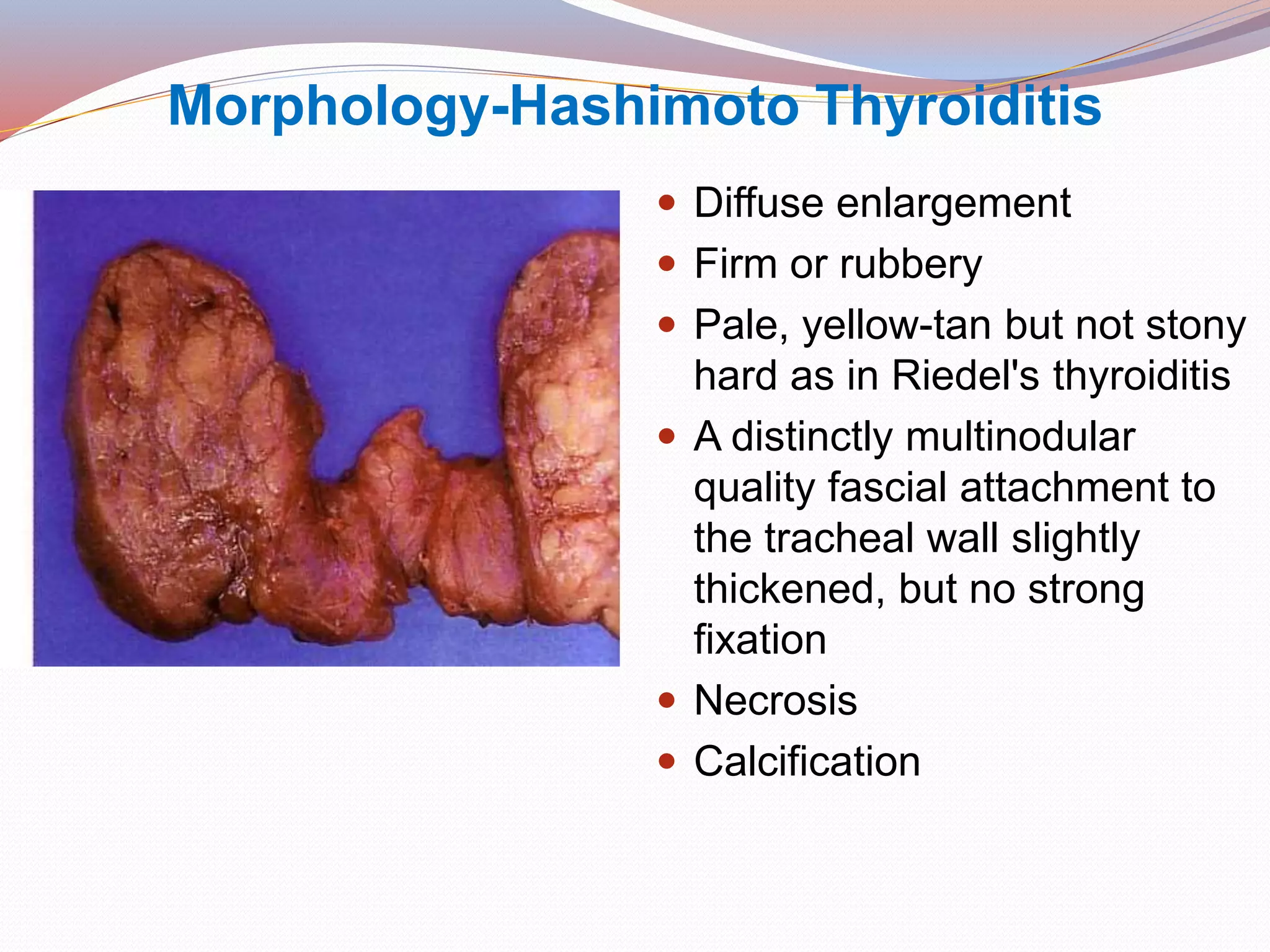
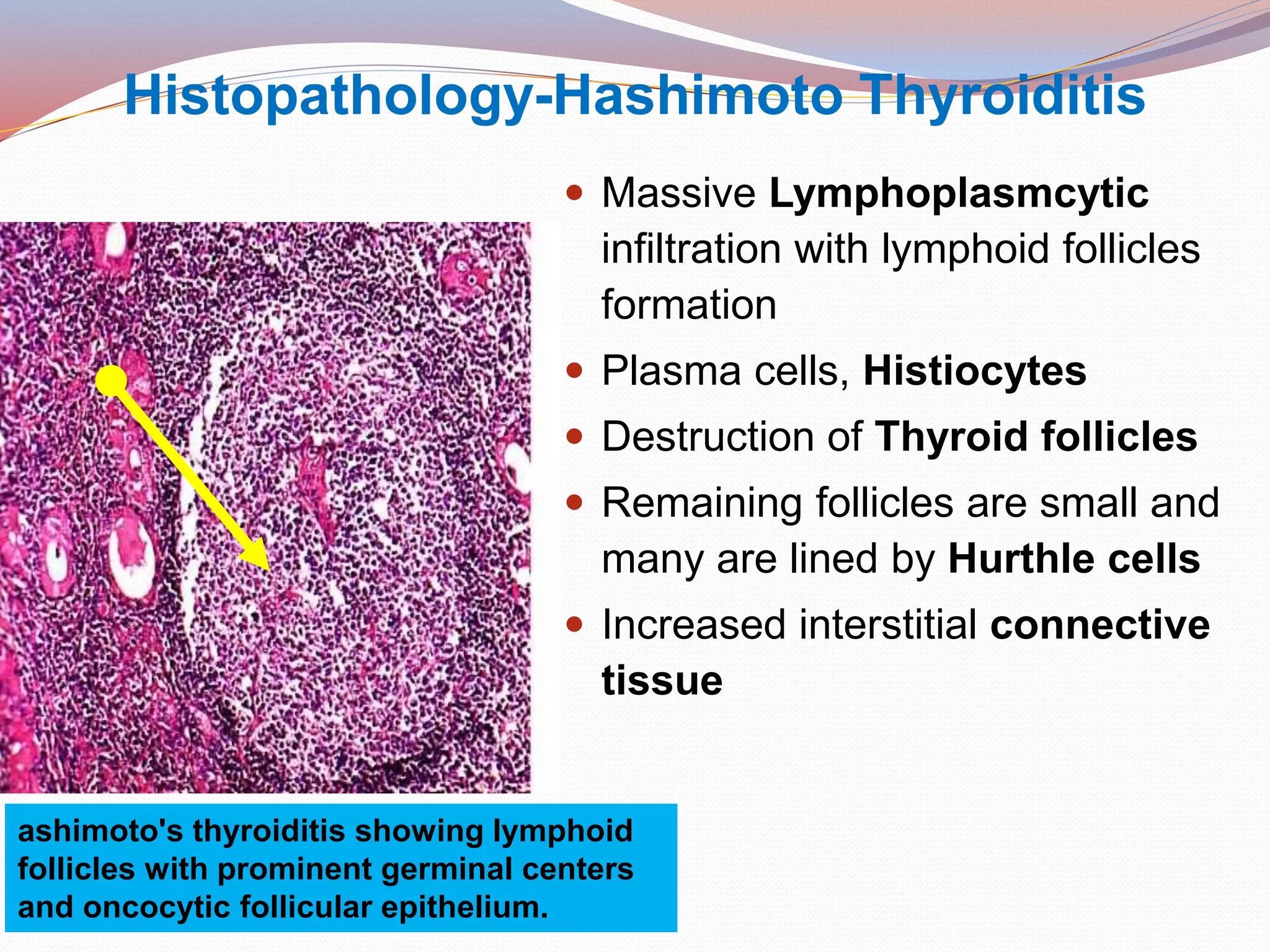
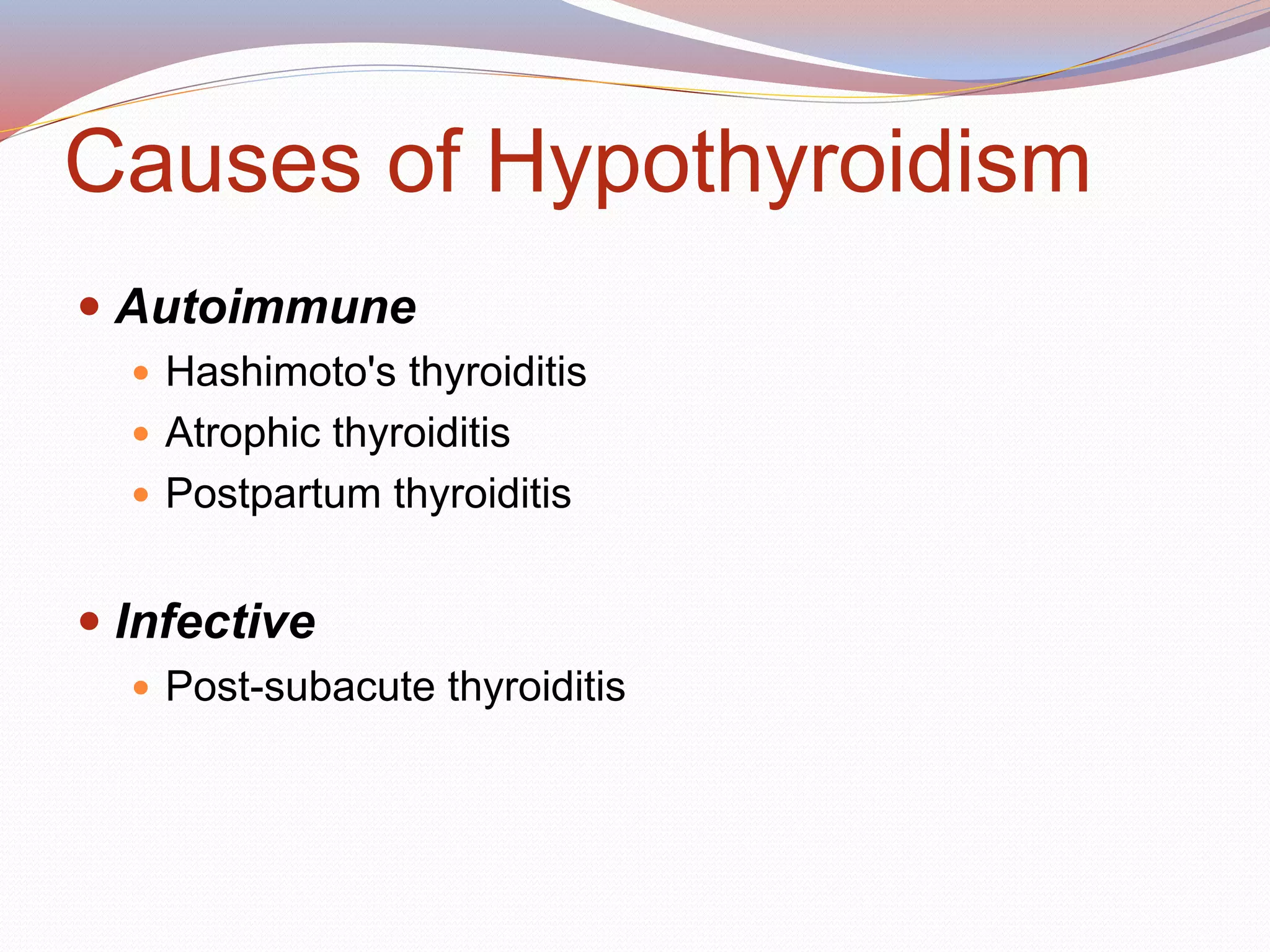
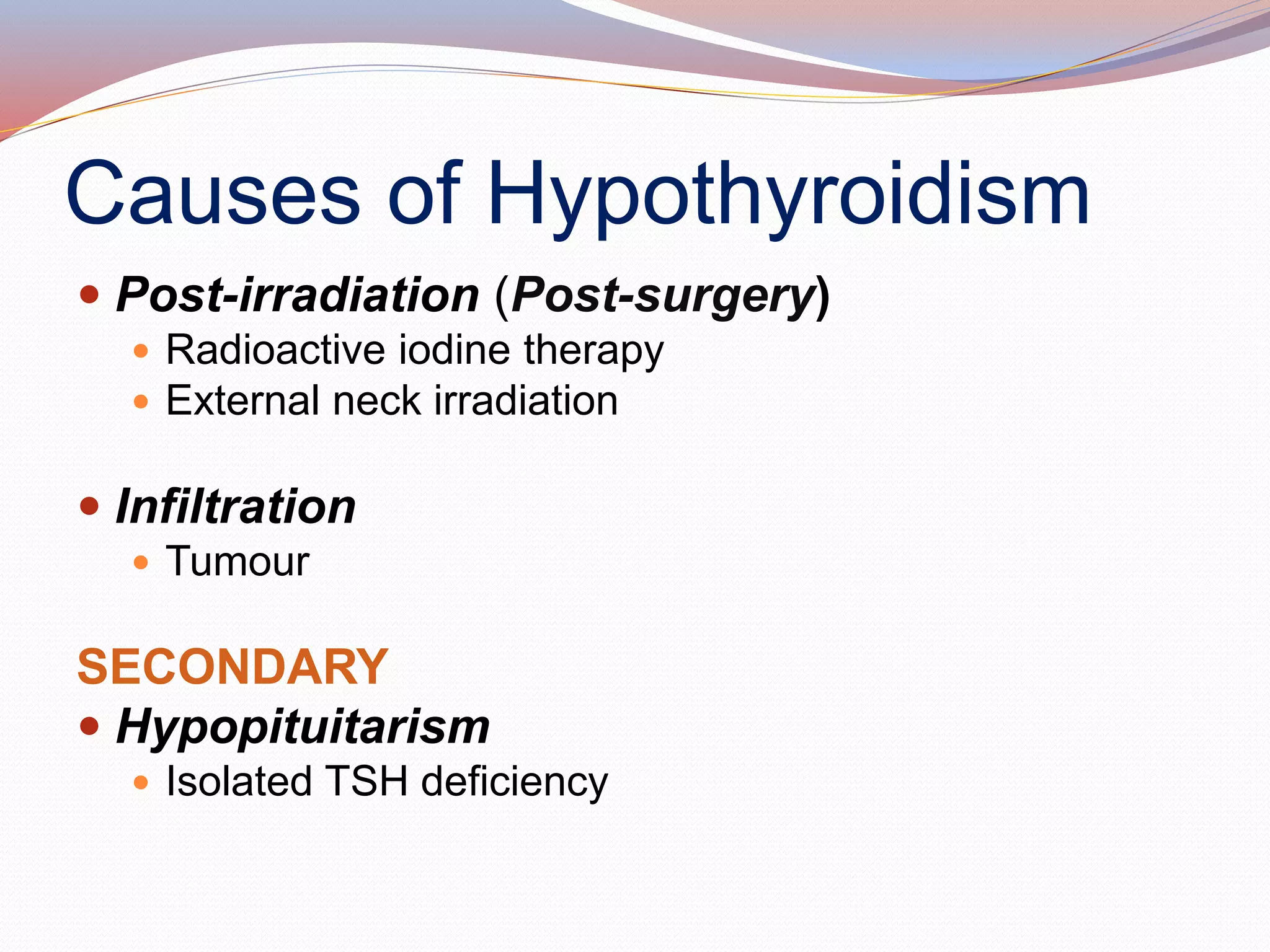
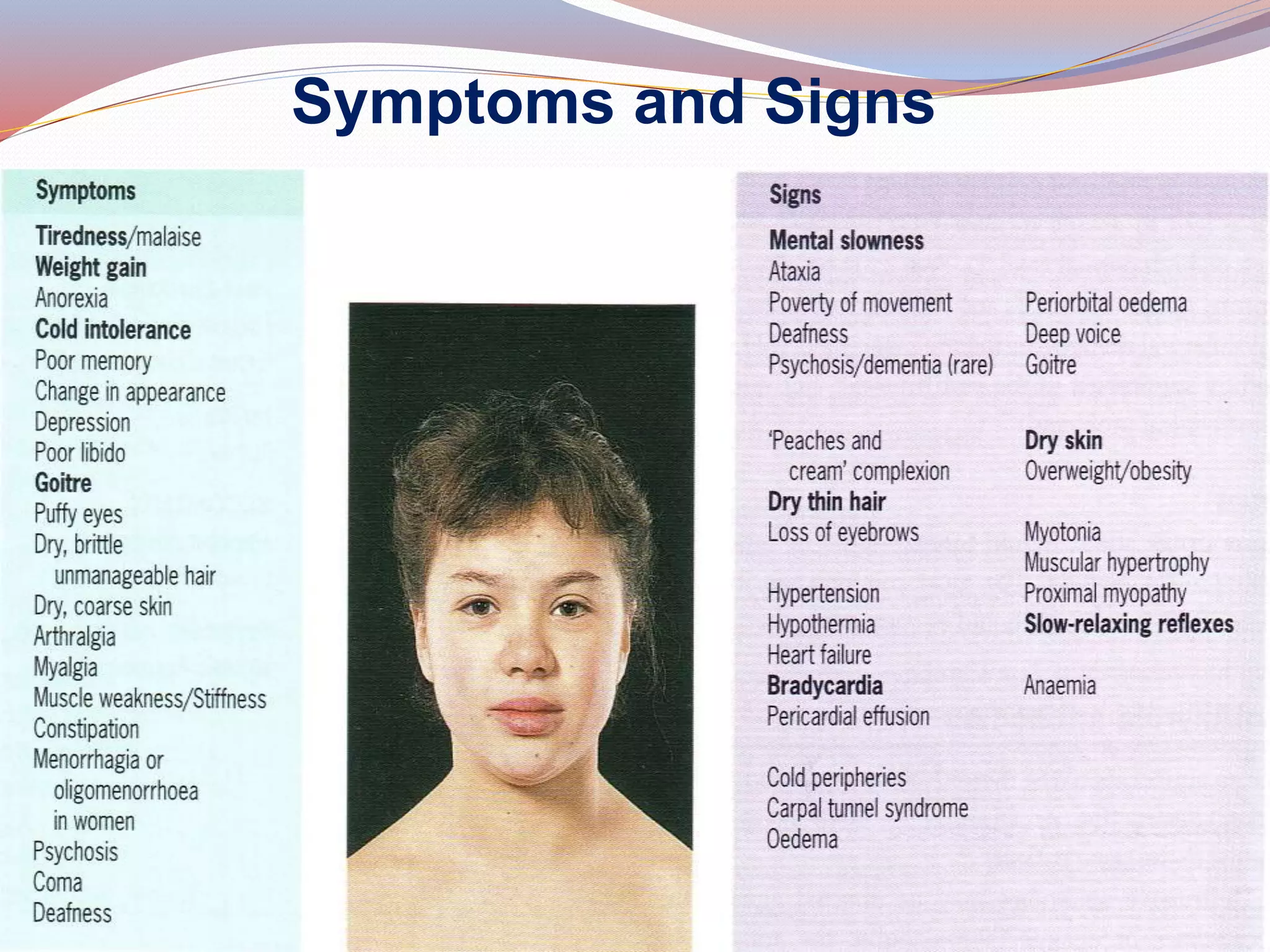
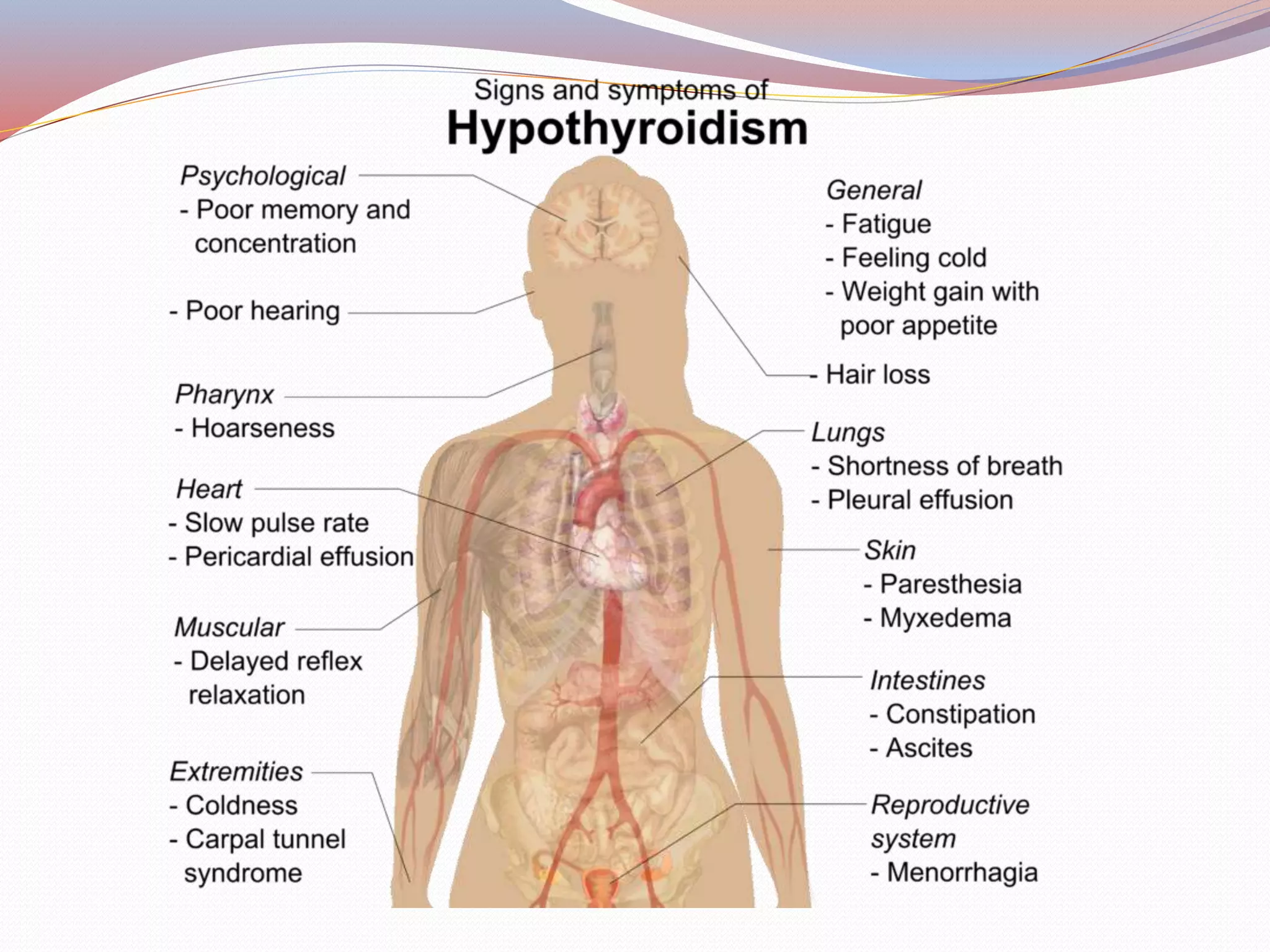
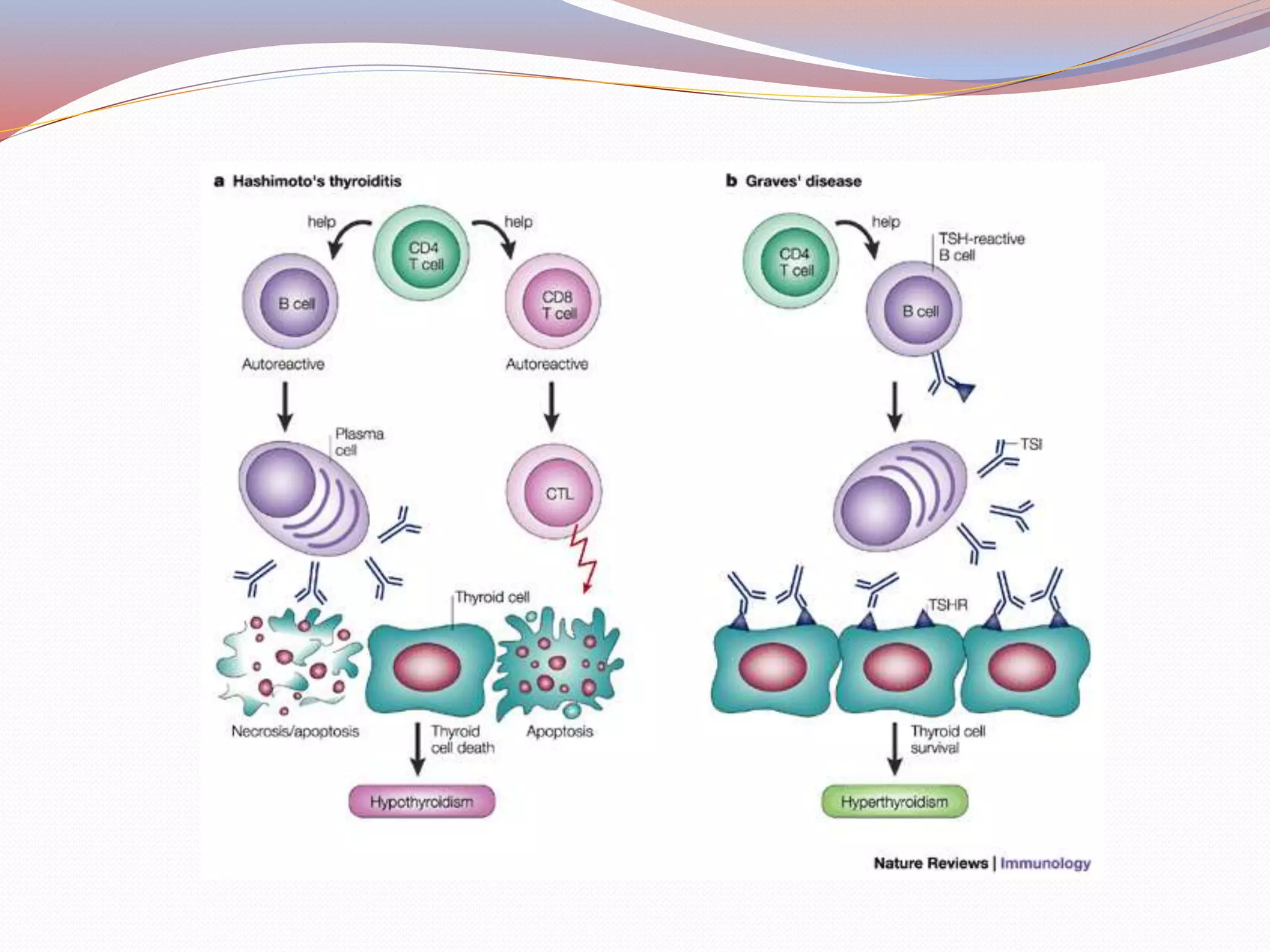
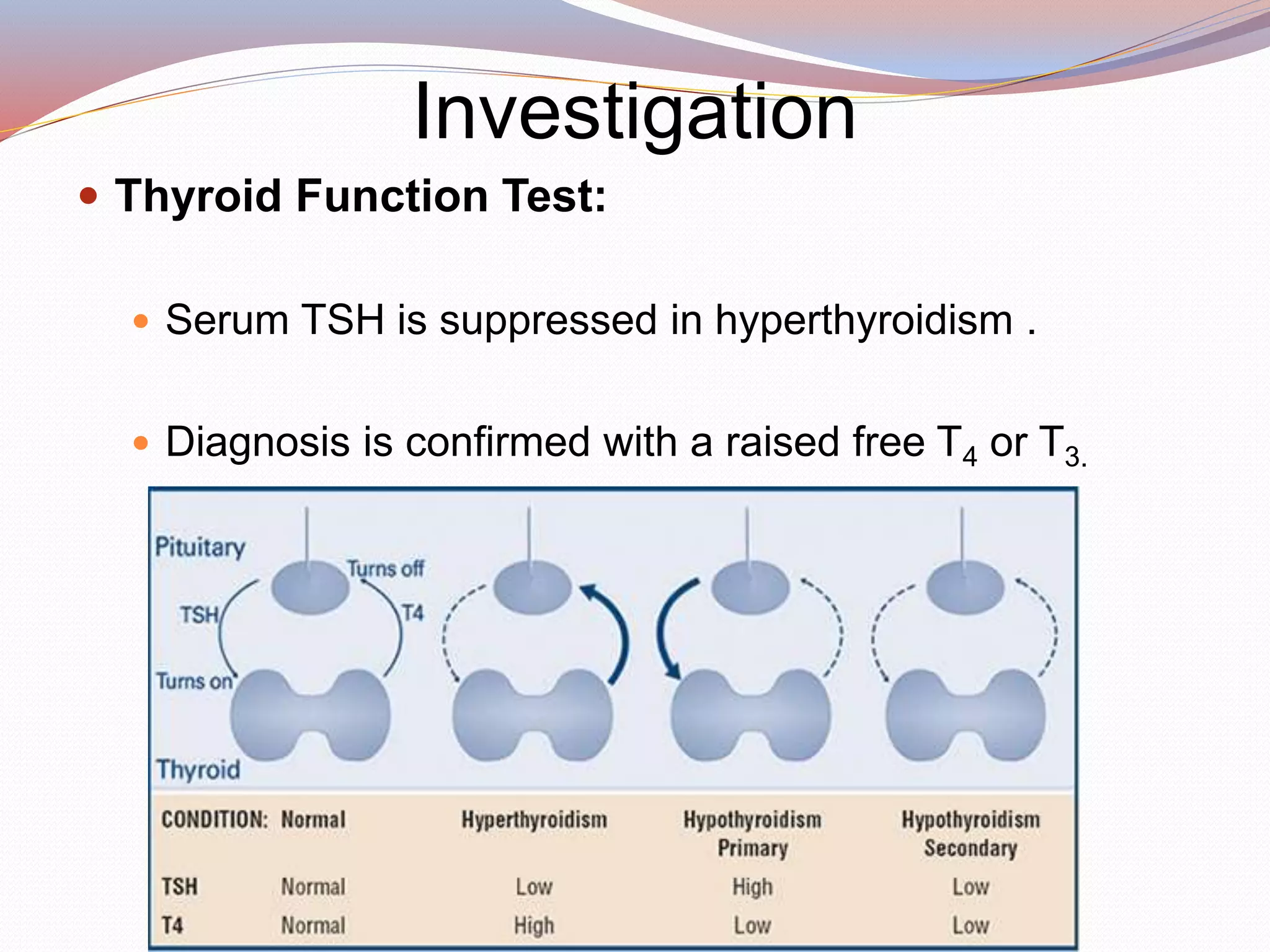
The thyroid gland regulates metabolism and plays a key role in many body functions. Hypothyroidism occurs when the thyroid gland is underactive and does not produce enough hormones. It can be caused by autoimmune diseases like Hashimoto's thyroiditis or problems with the pituitary gland. Symptoms include fatigue, weight gain, dry skin and hair, and feeling cold. Blood tests are used to diagnose hypothyroidism by measuring thyroid stimulating hormone and thyroid hormone levels. Lifelong thyroid hormone replacement therapy is needed to treat hypothyroidism and prevent serious complications like myxedema coma.