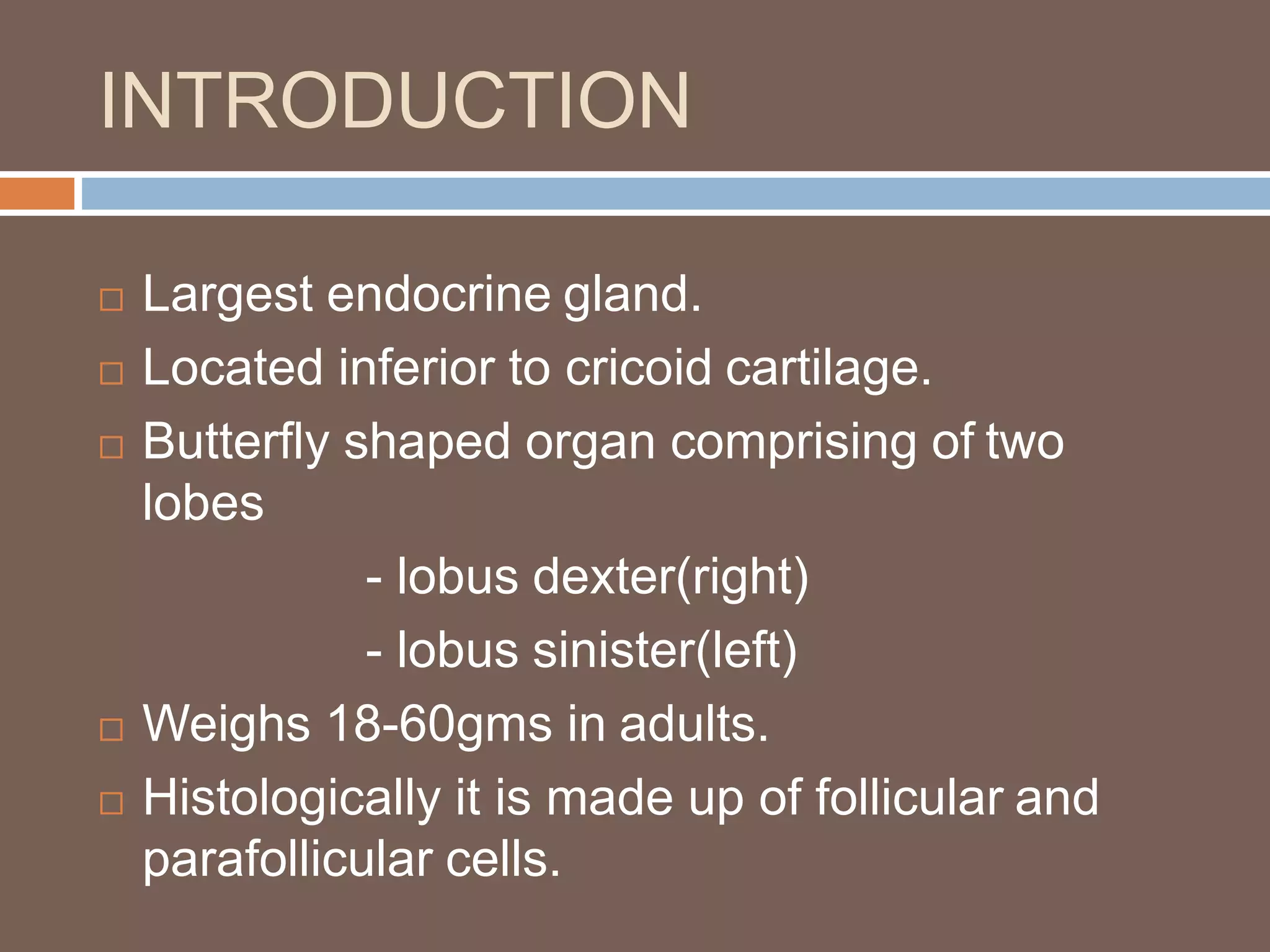
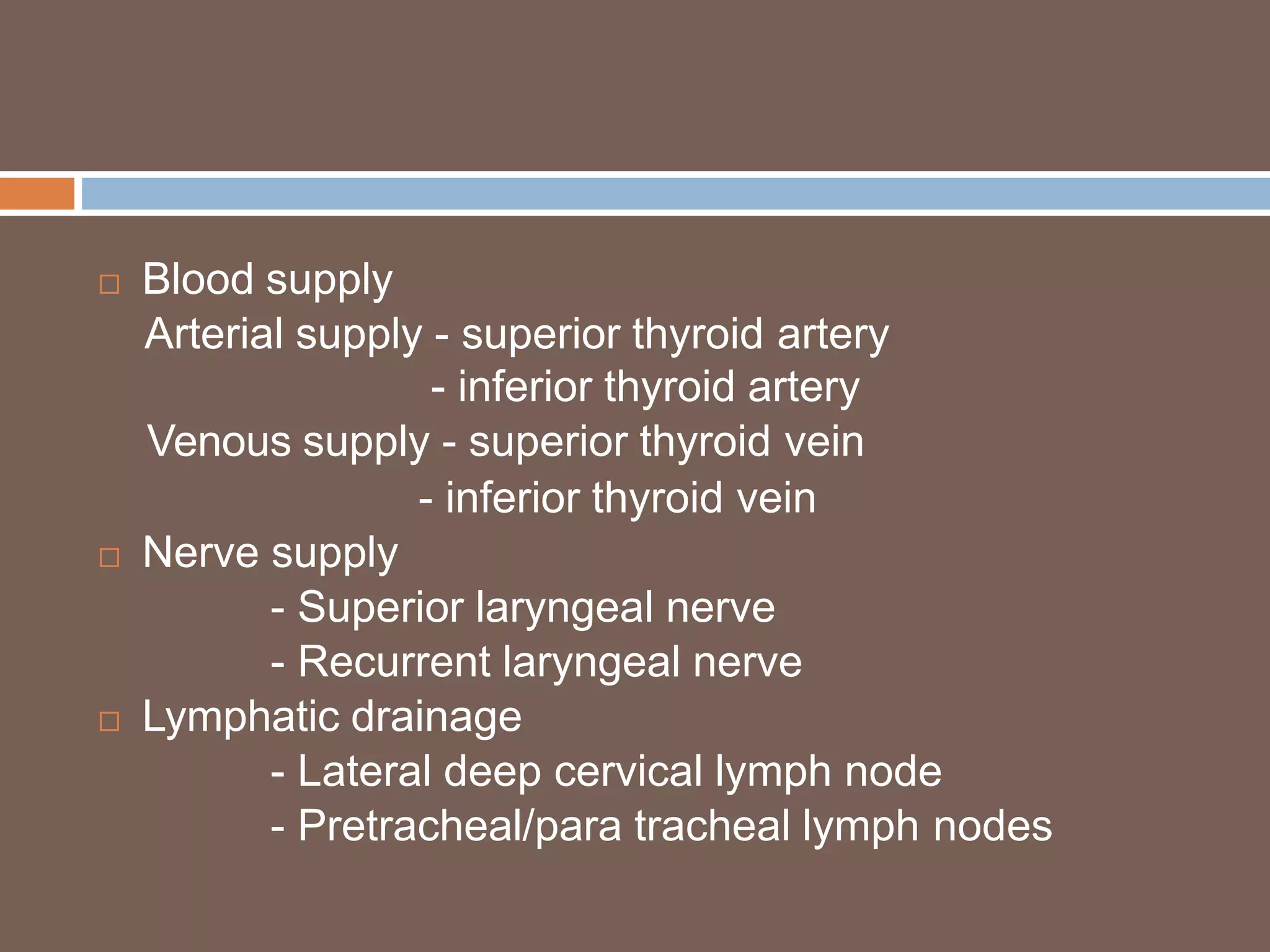
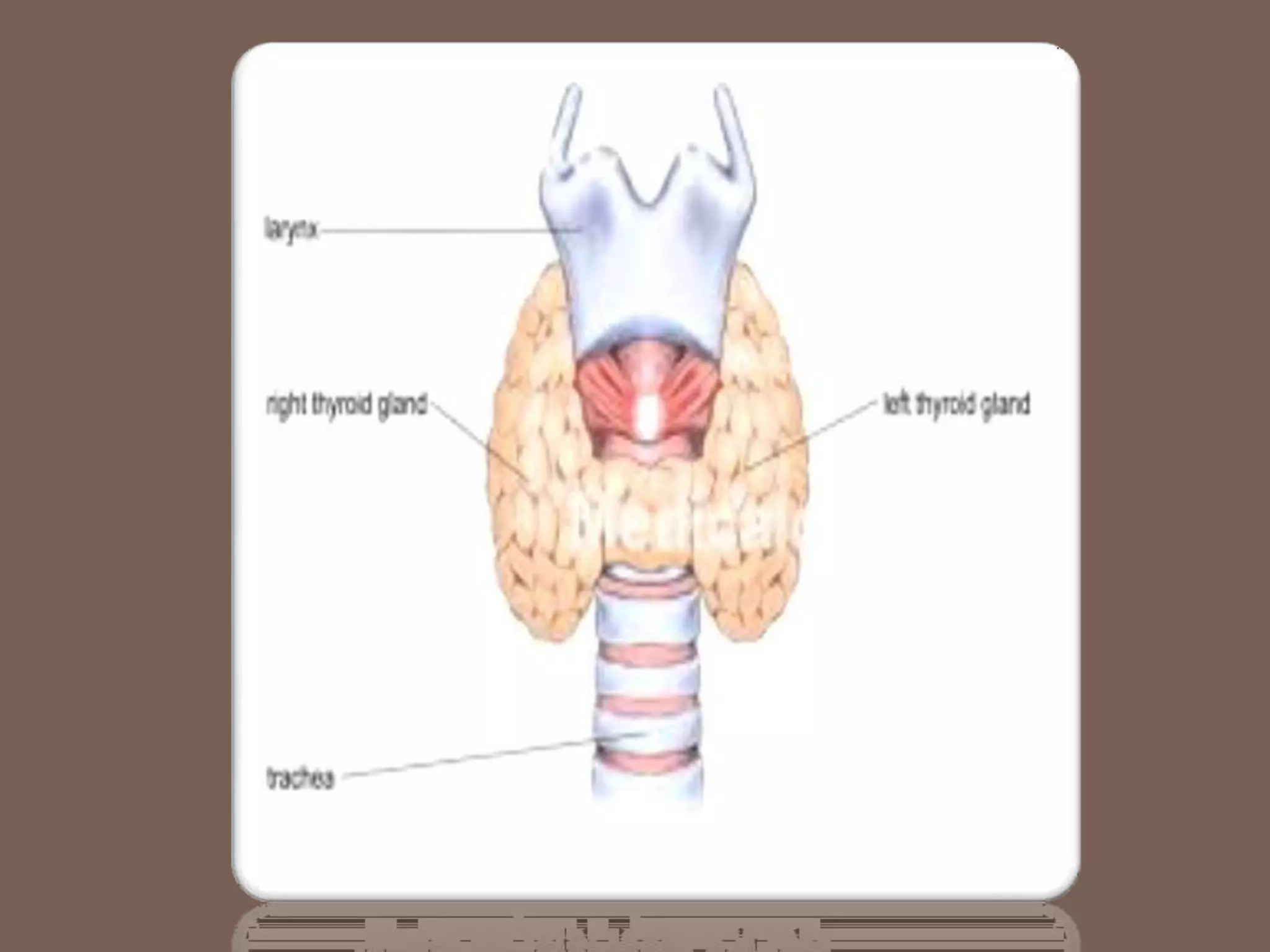
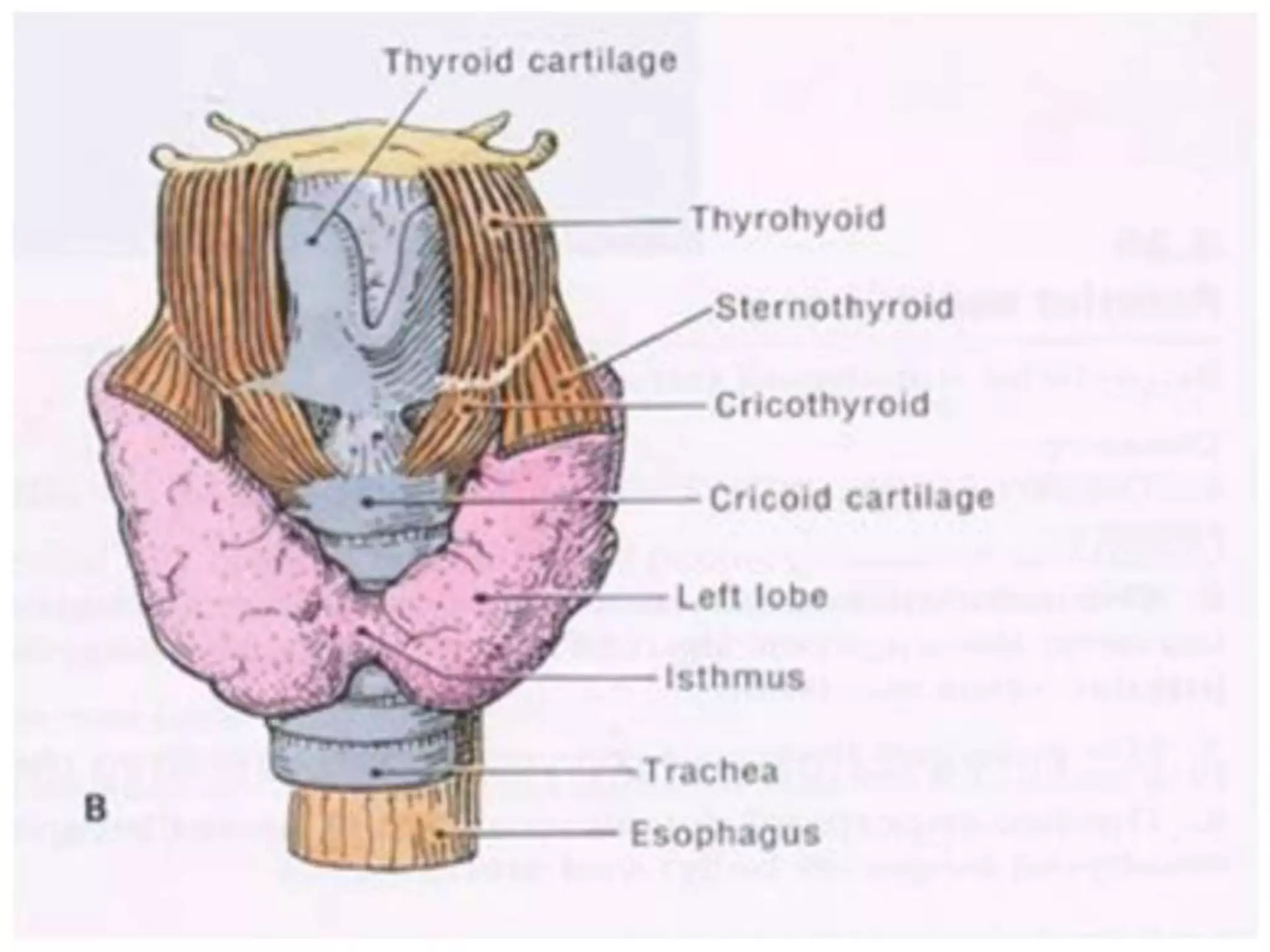
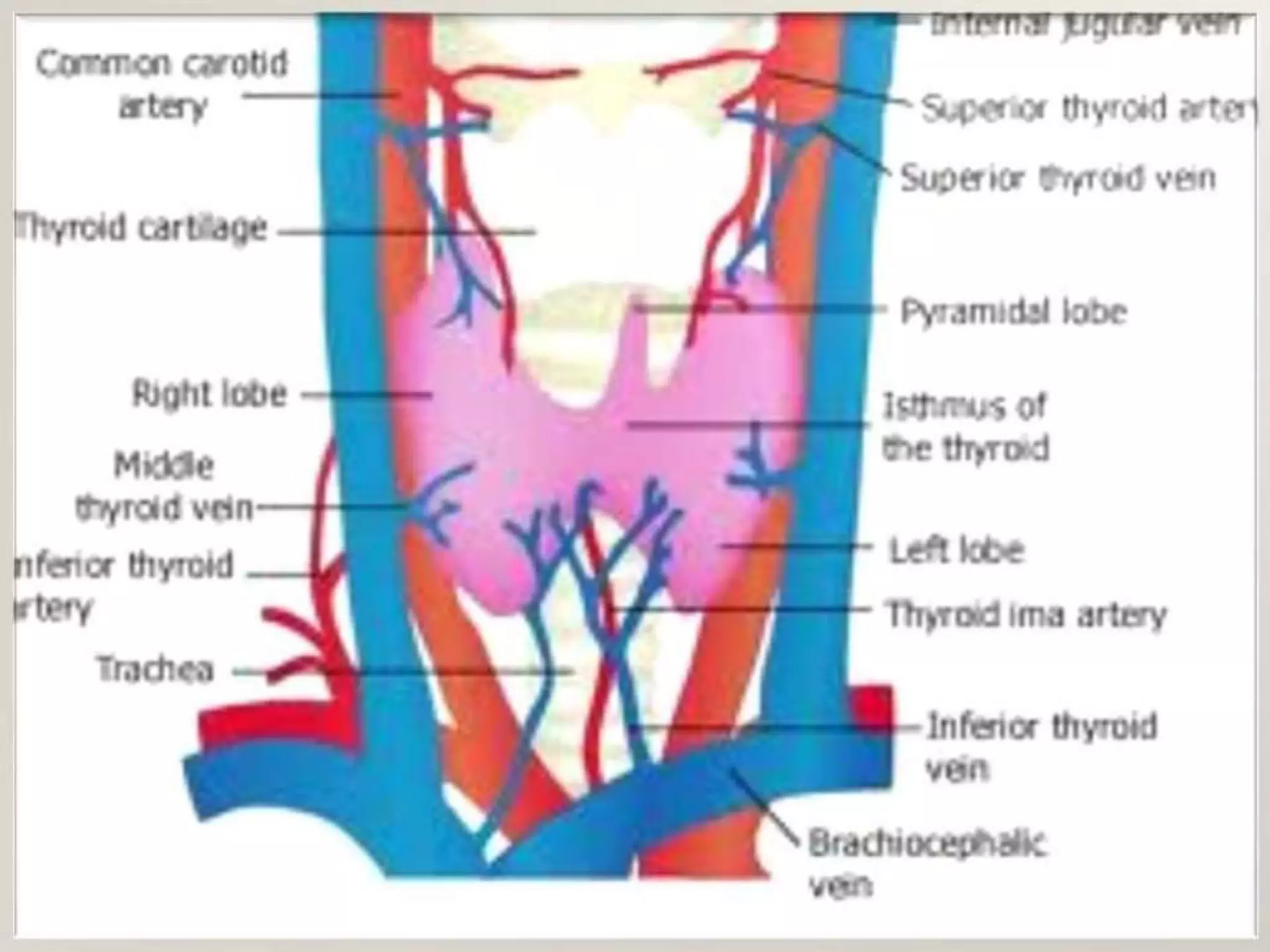
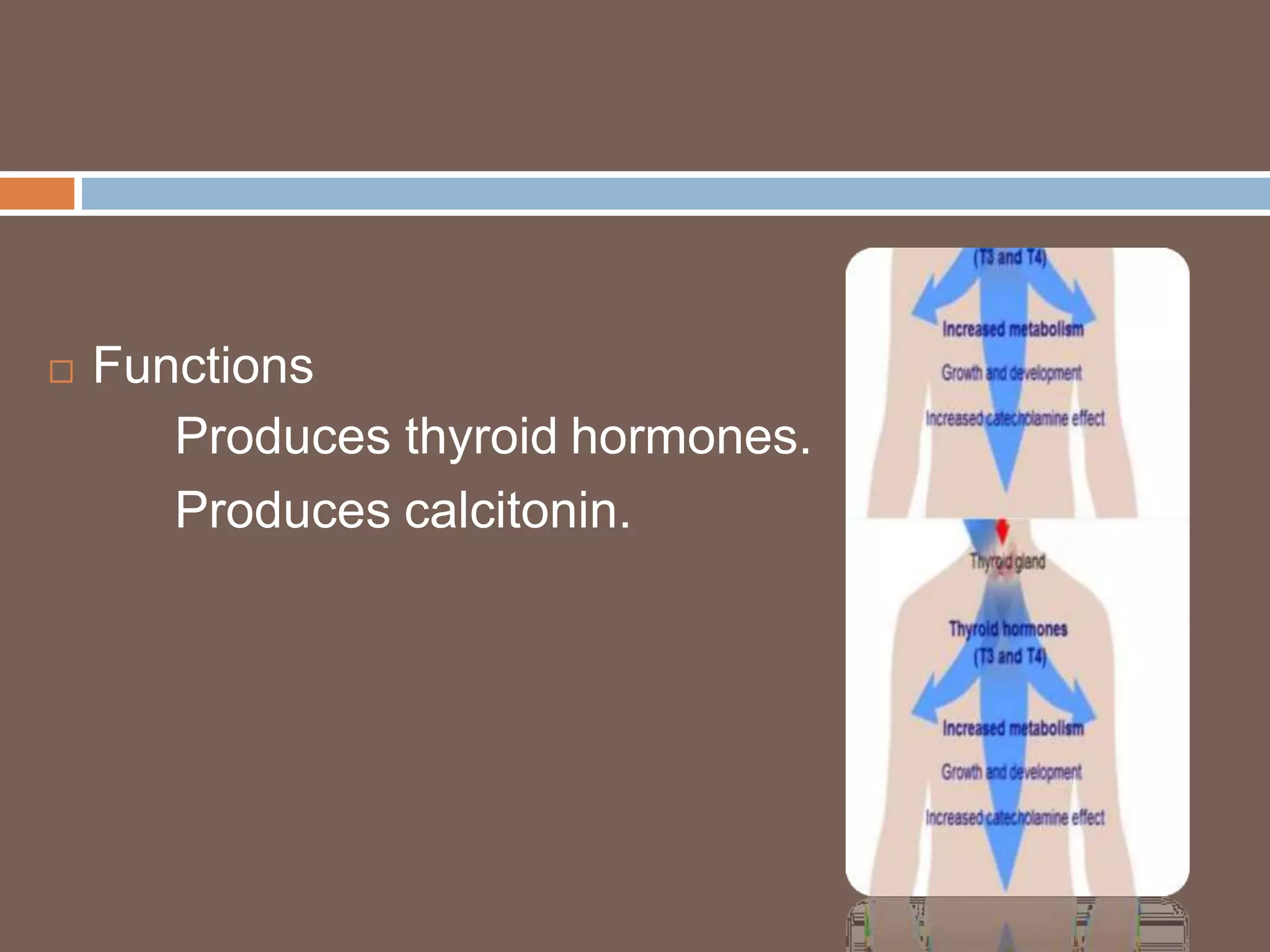
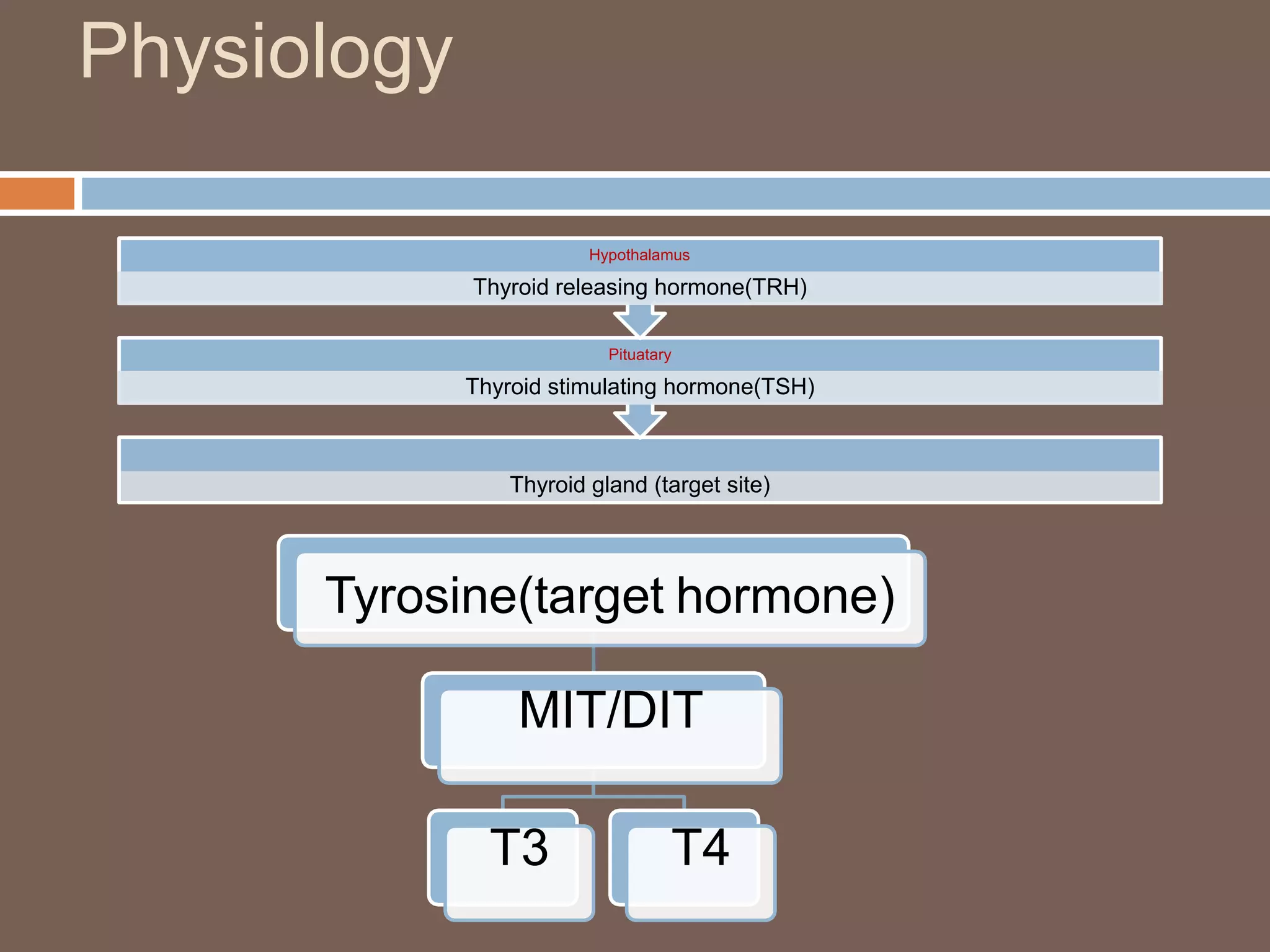
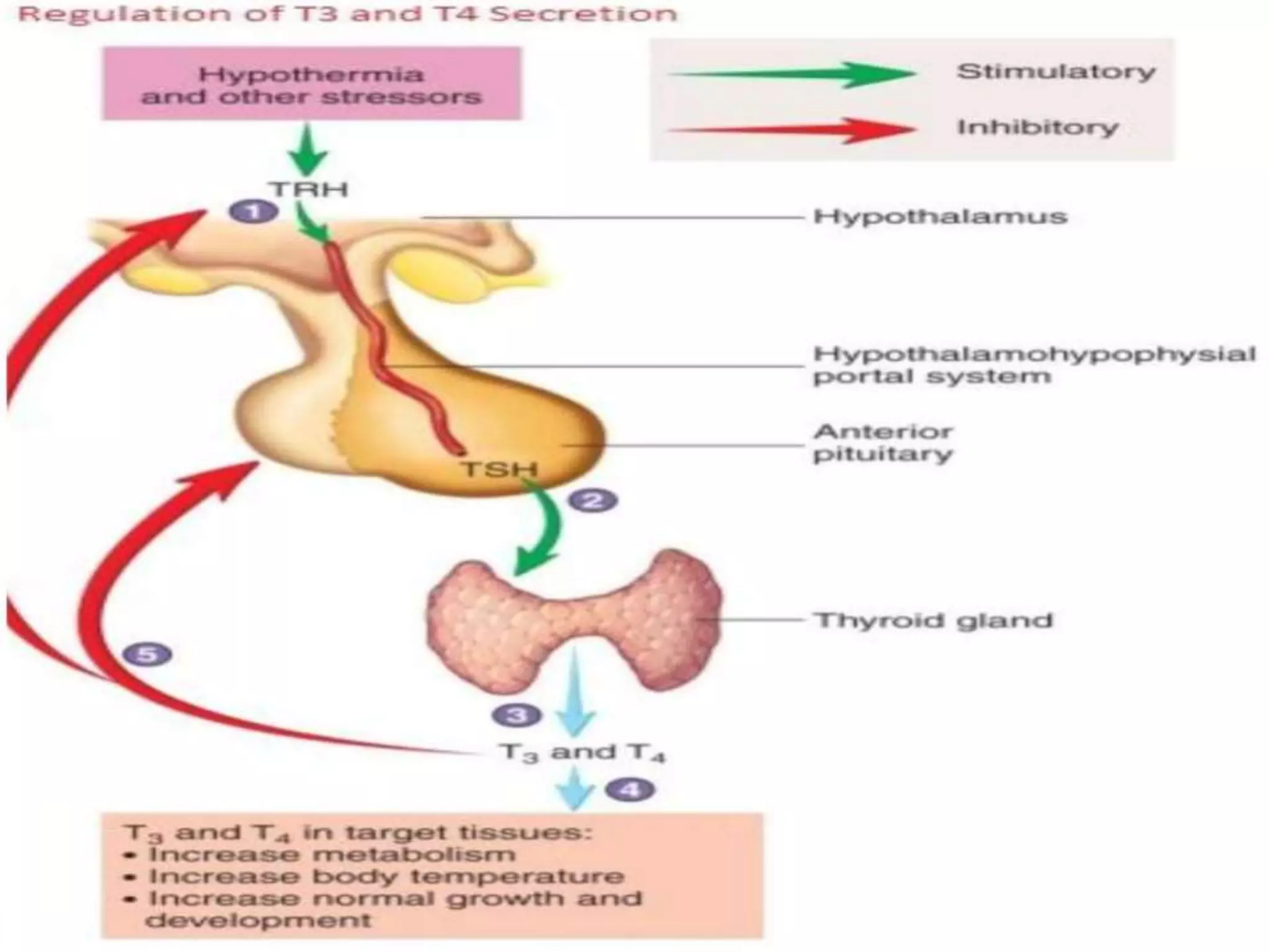
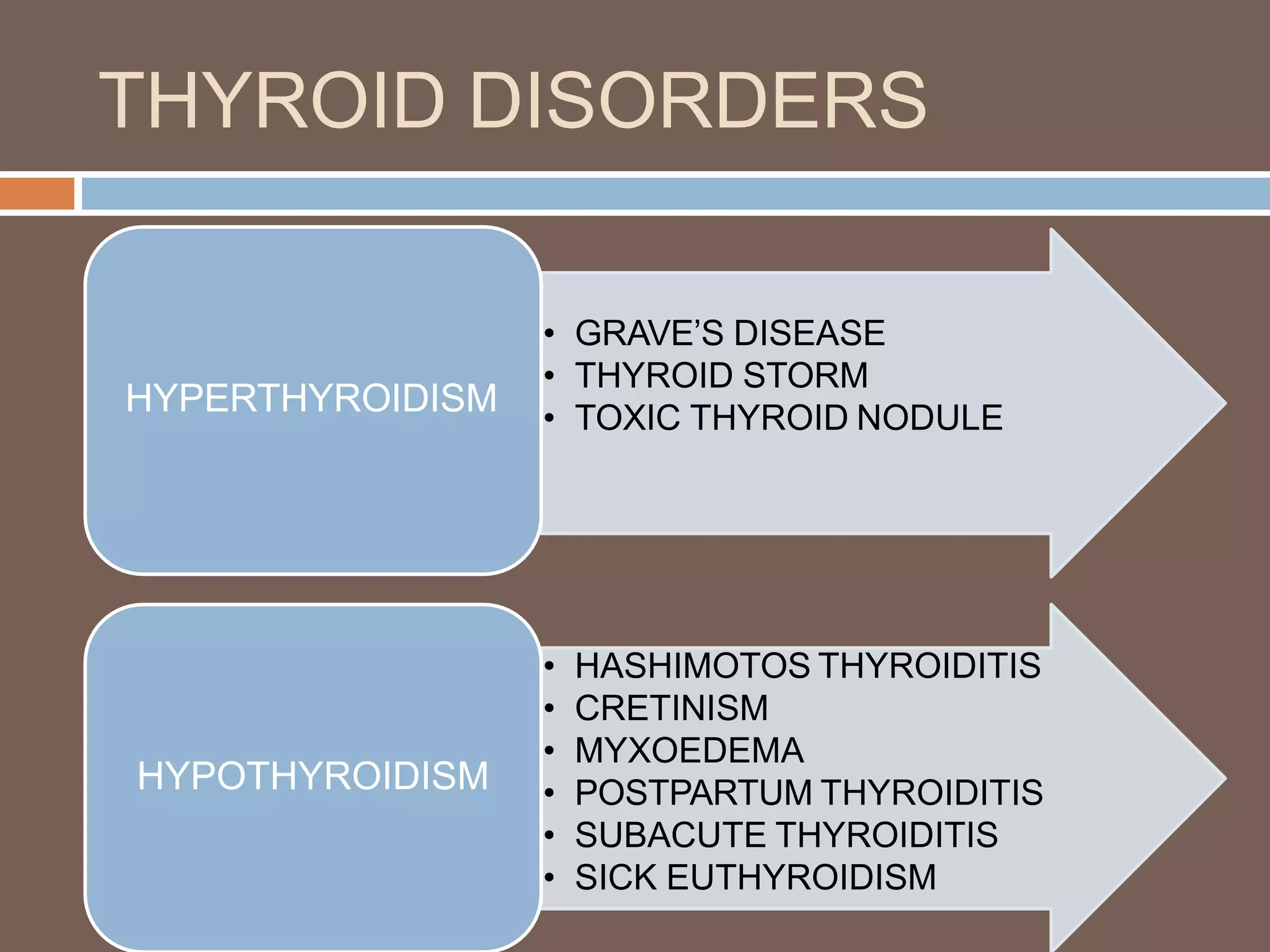
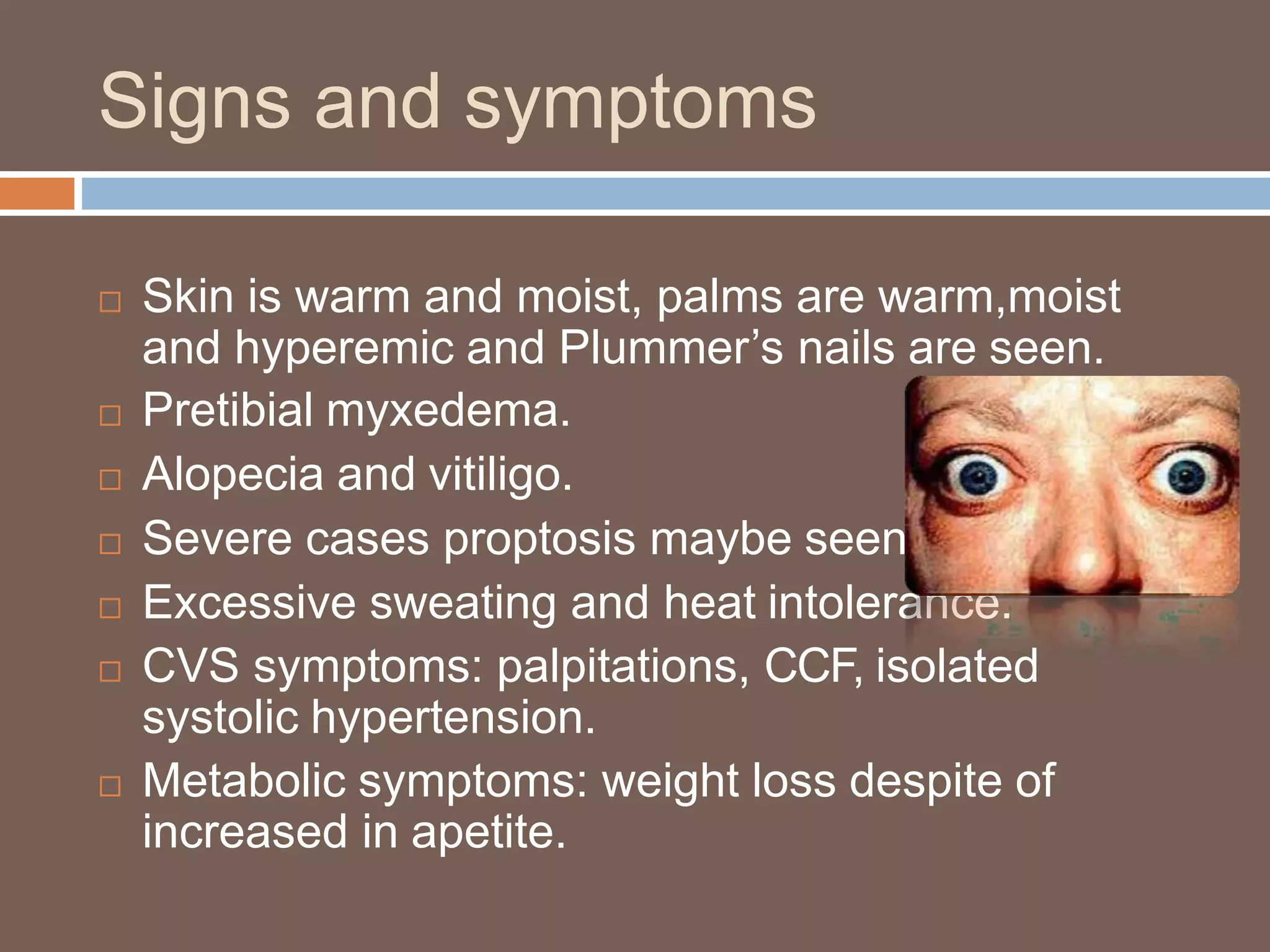
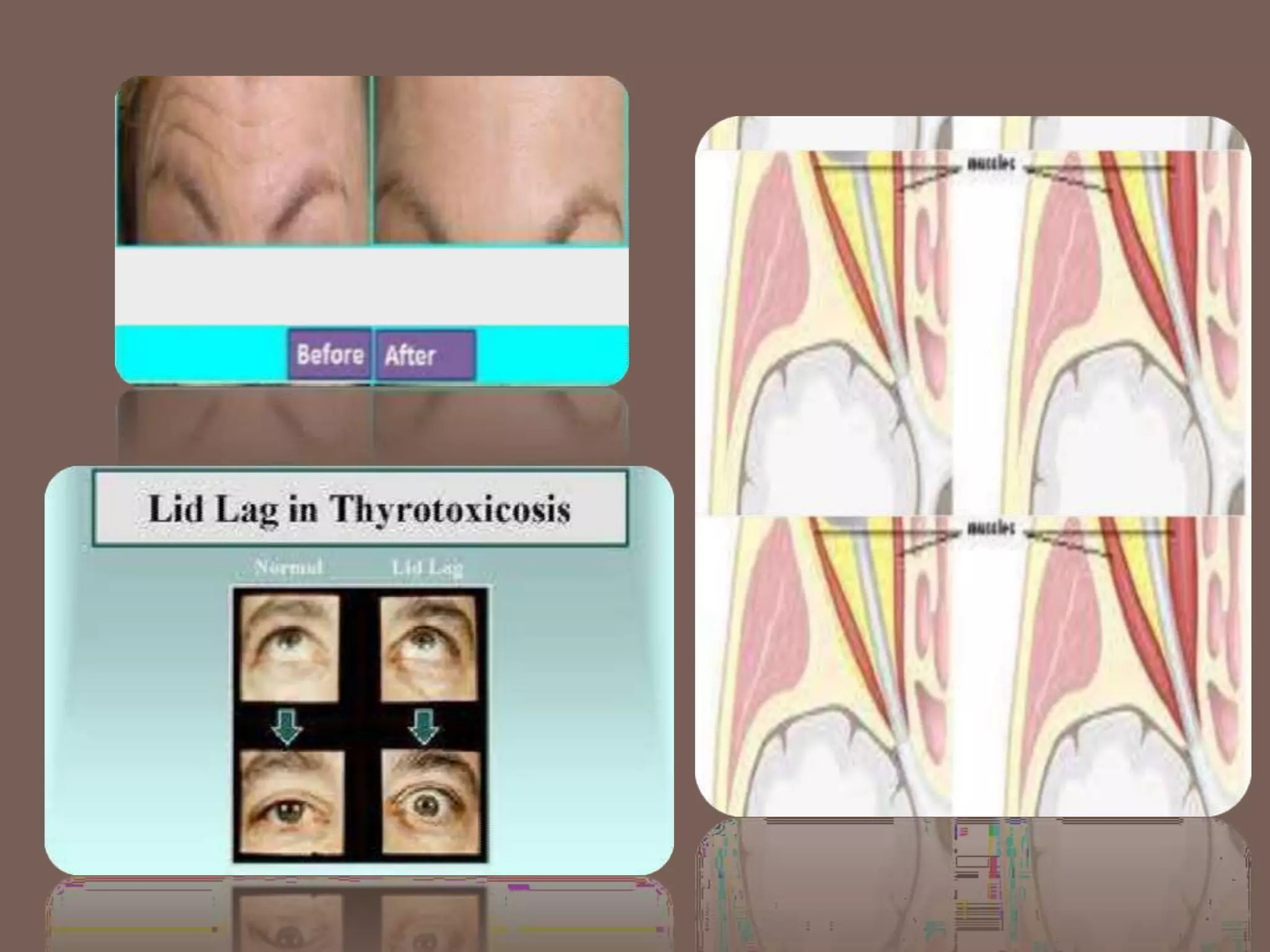
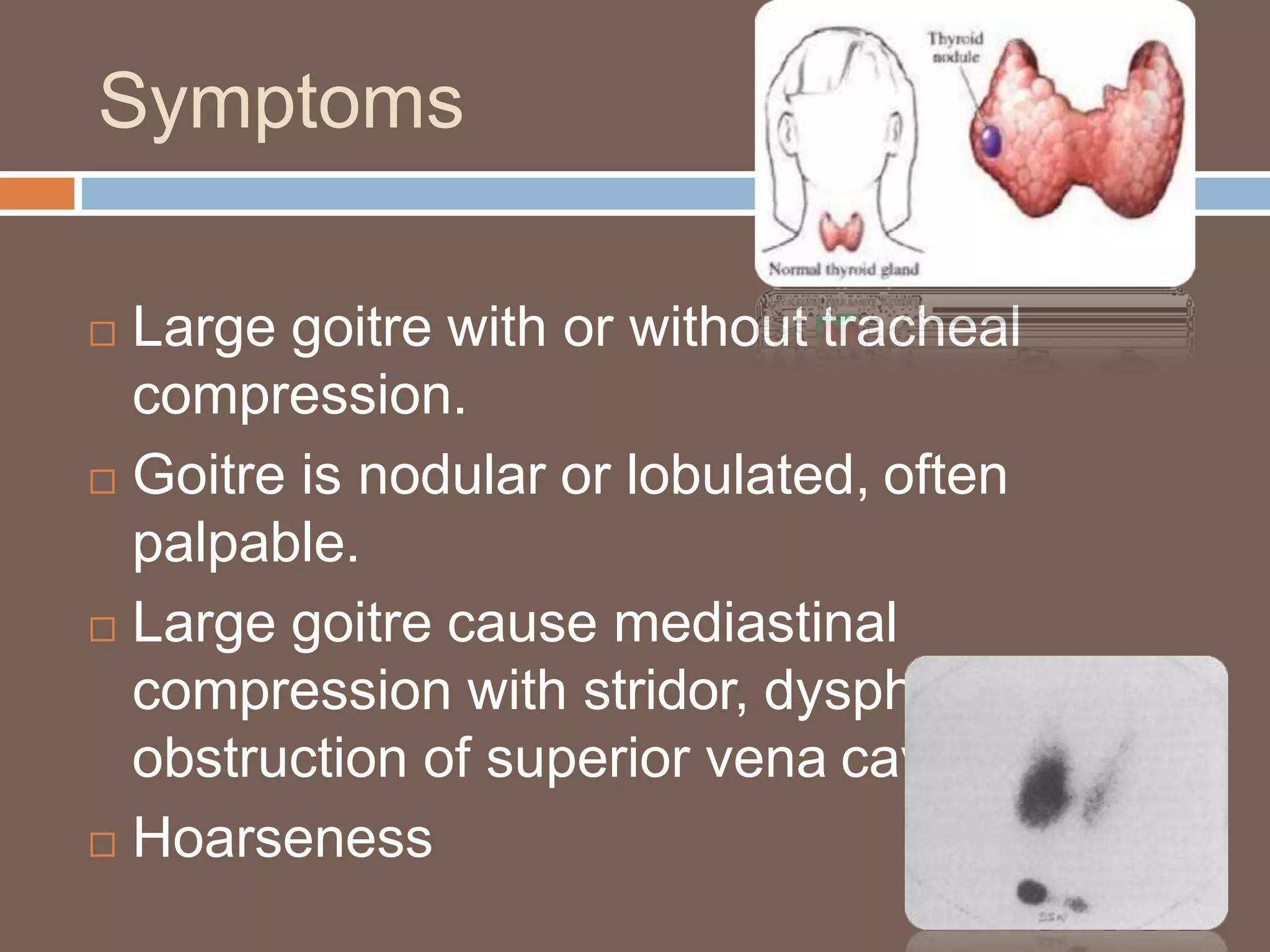
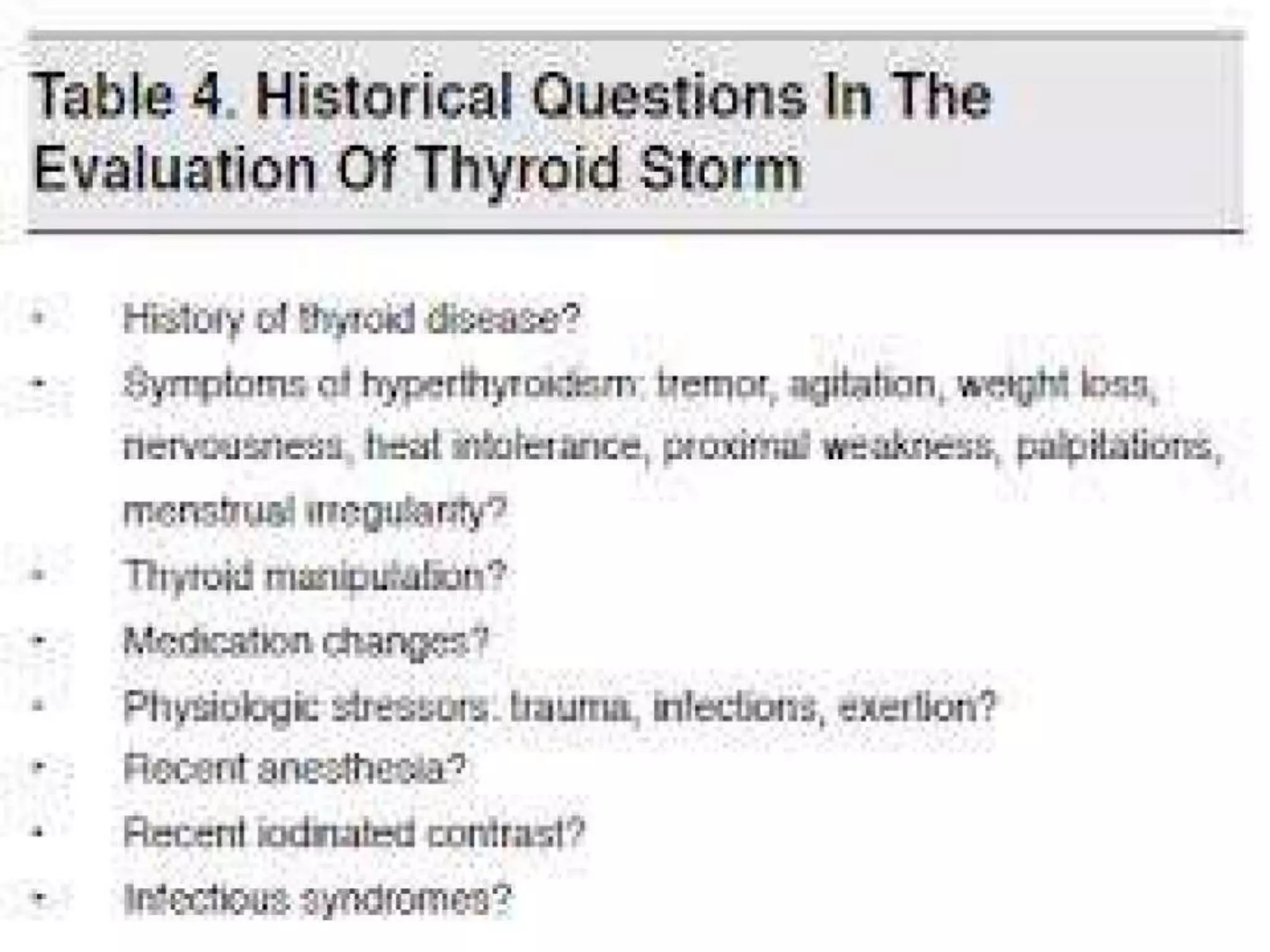
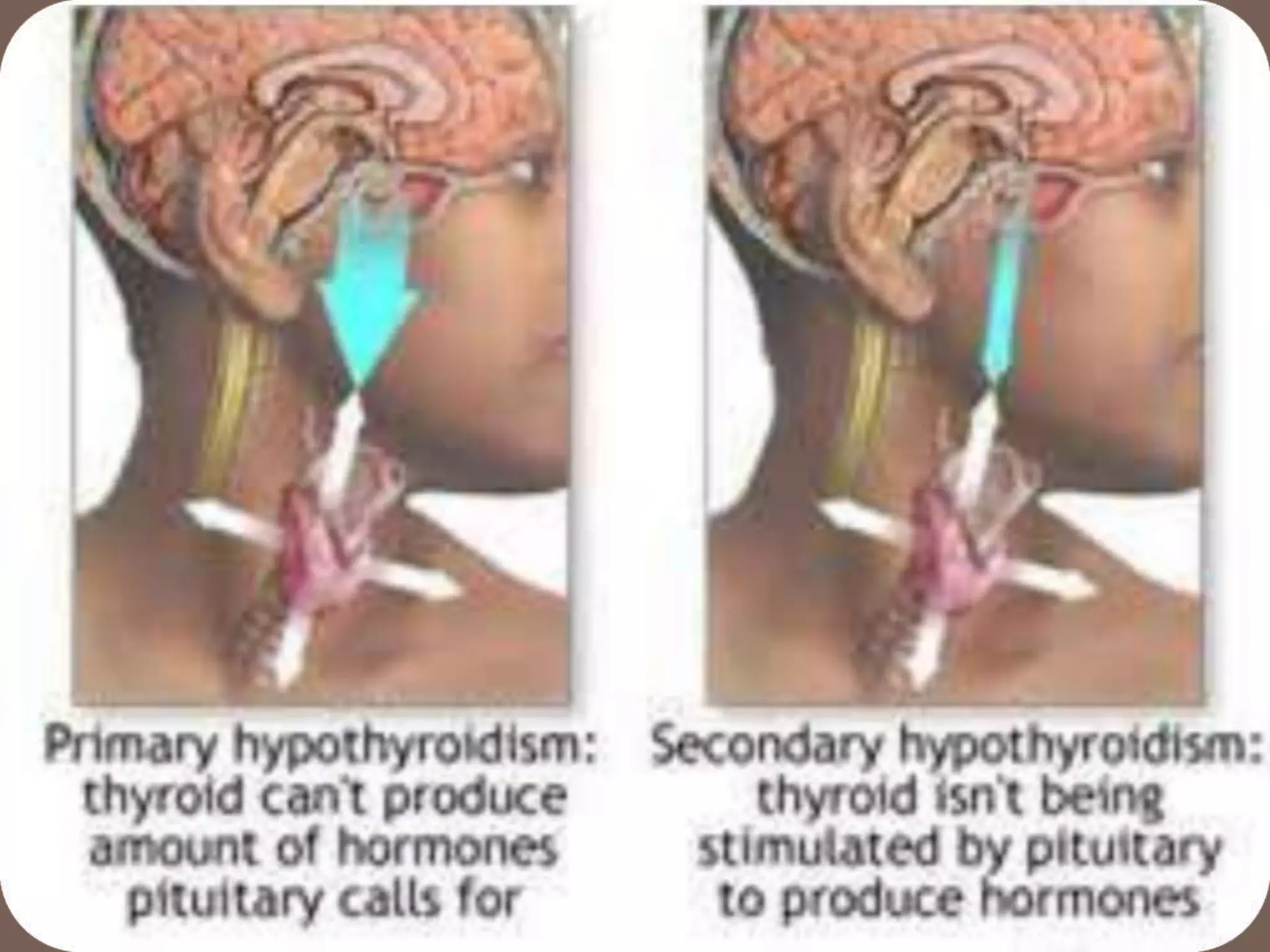
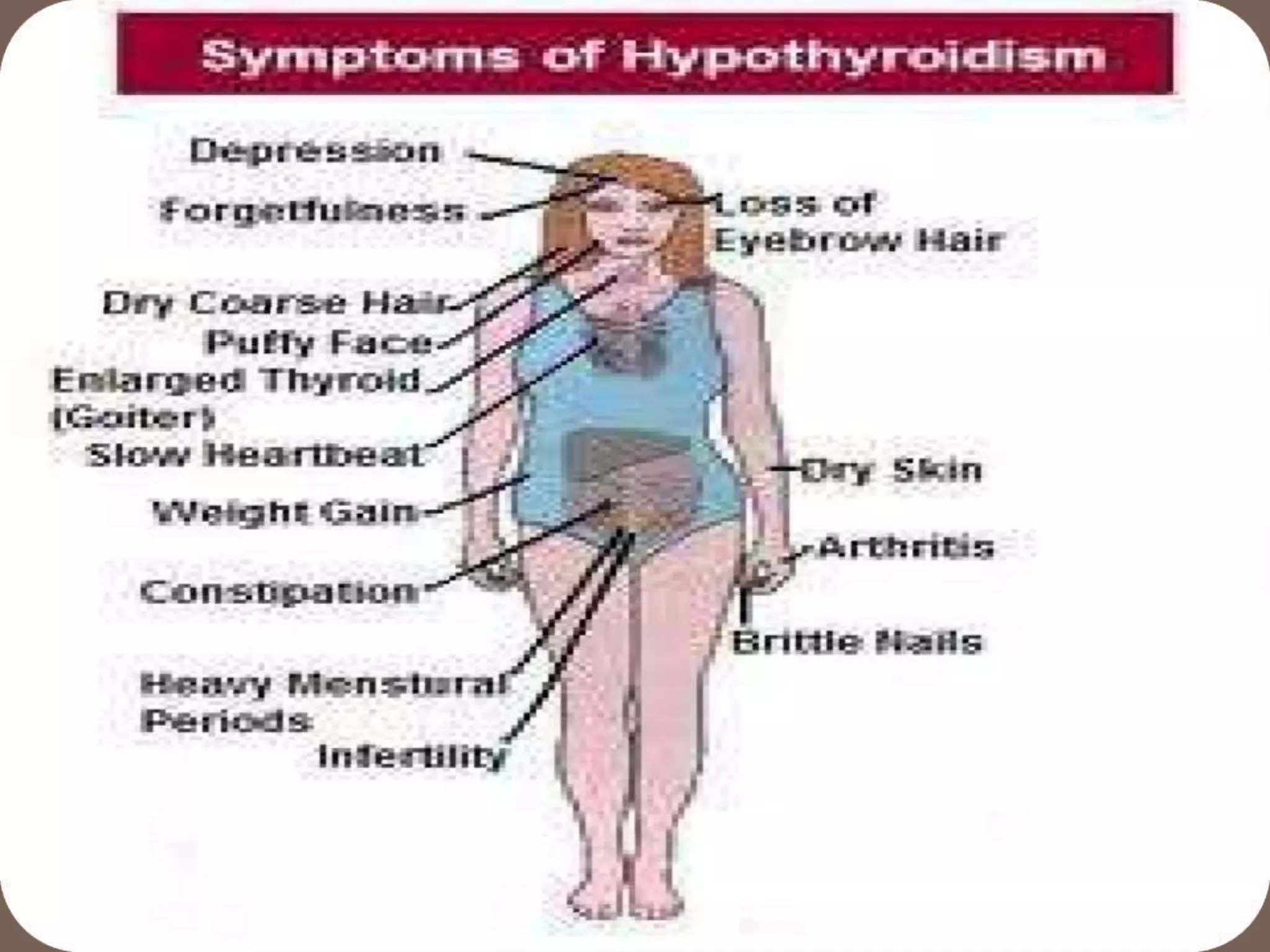
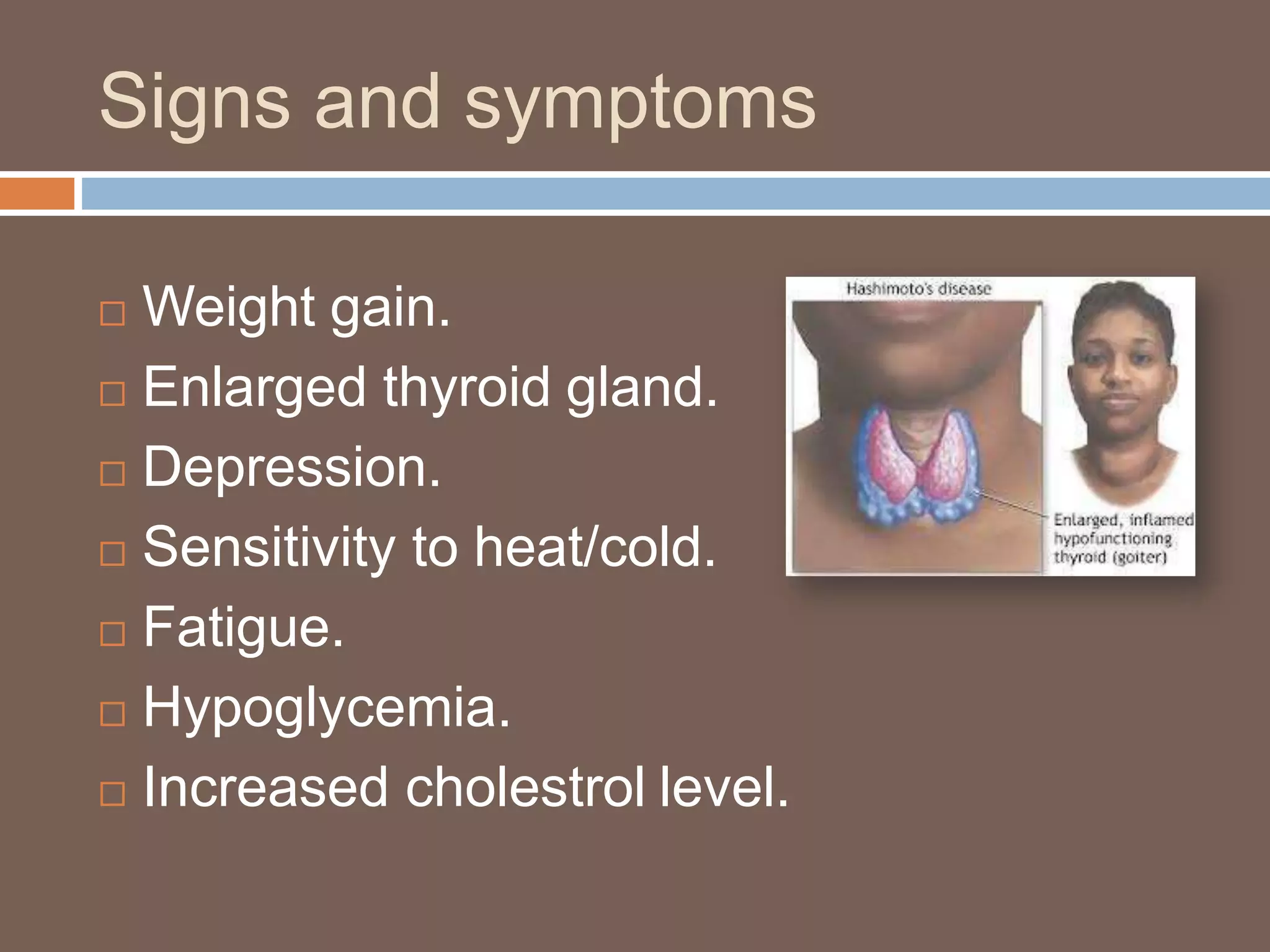
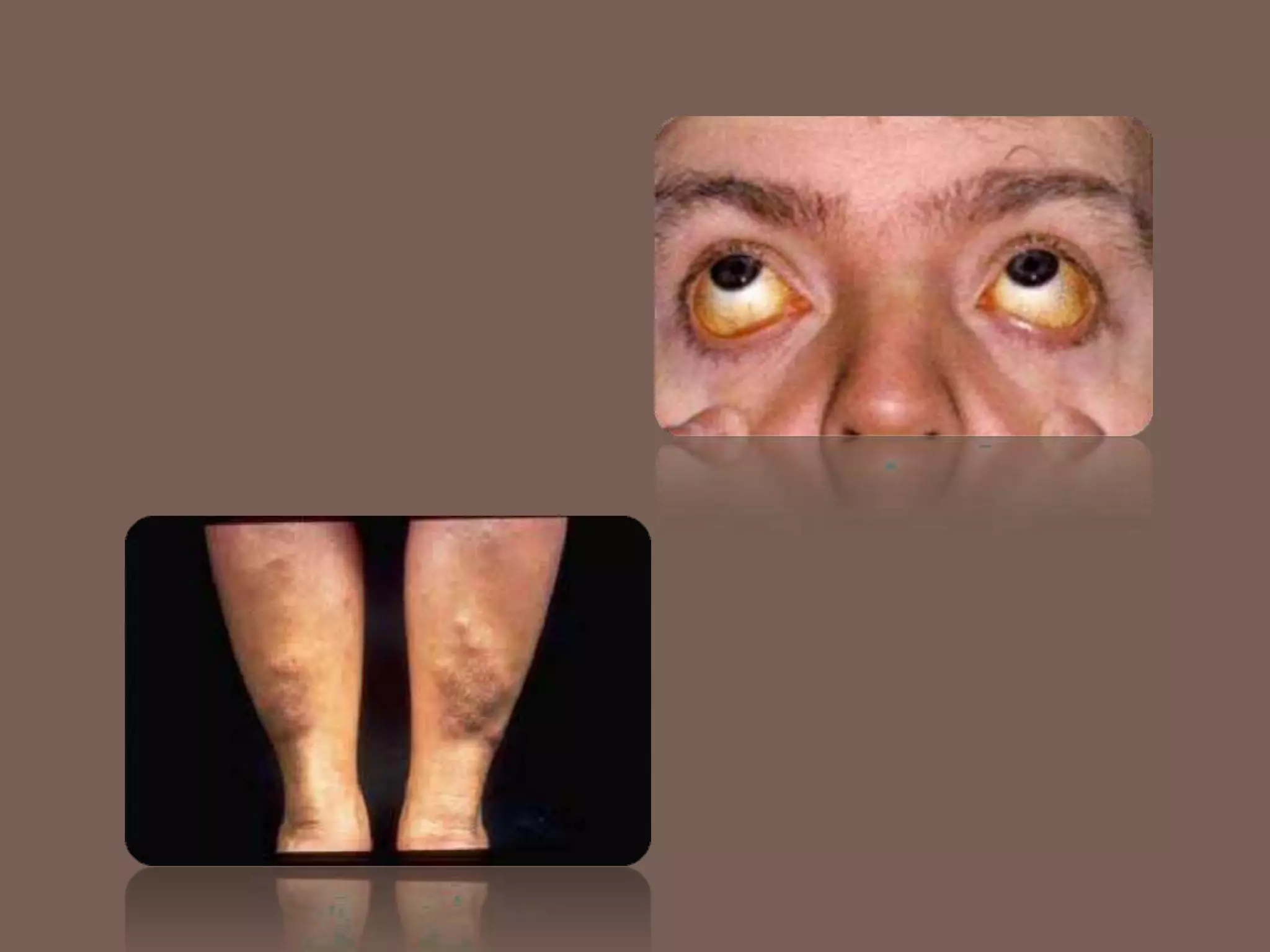
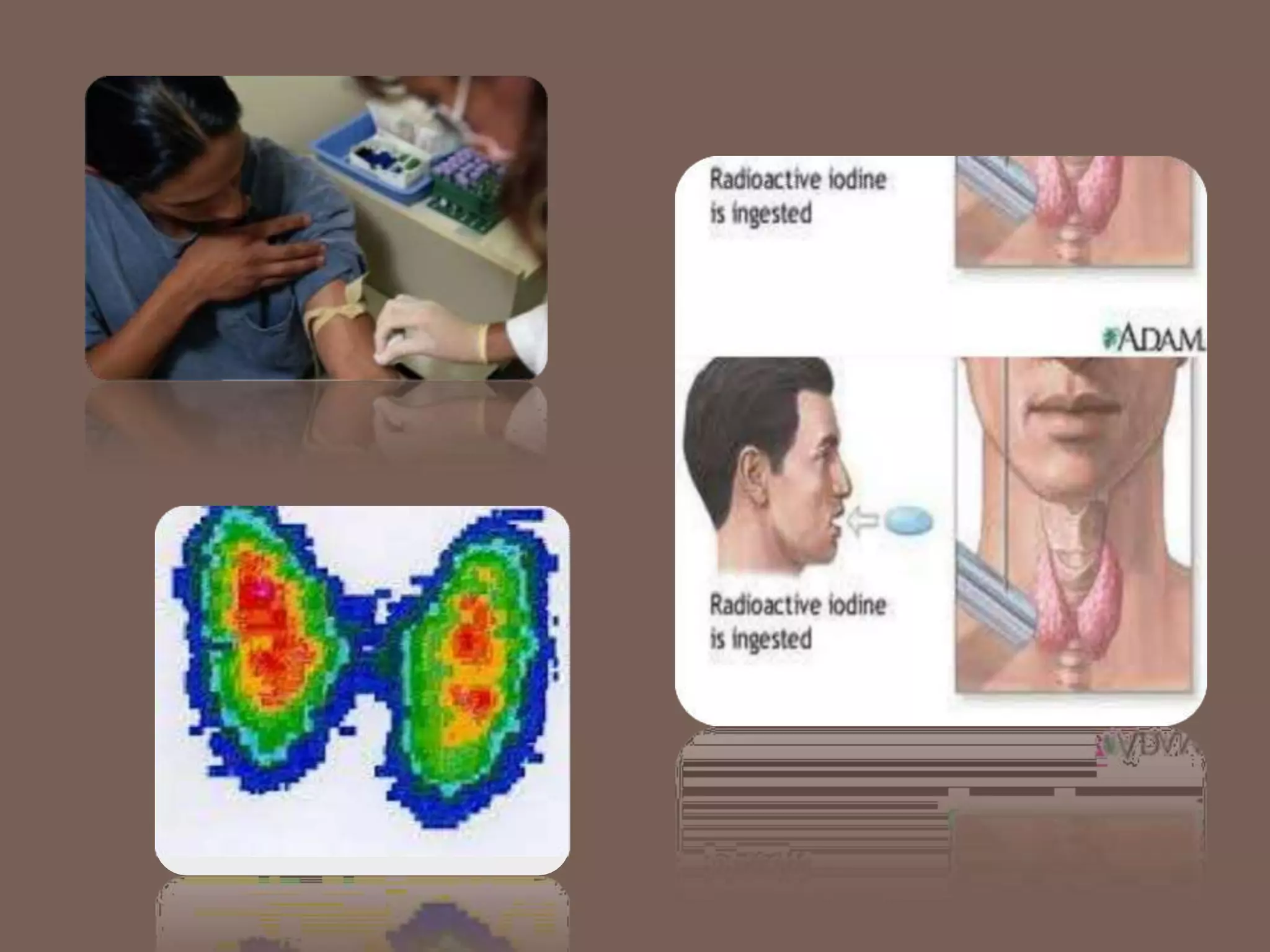
The document provides an overview of thyroid disorders, detailing the anatomy, physiology, and various conditions affecting the thyroid gland, such as Graves' disease, hypothyroidism, and cretinism. It discusses symptoms, diagnostic methods, and management strategies for each disorder, emphasizing the importance of thyroid hormone levels and treatment options like medication and surgery. The document highlights the critical nature of thyroid health and the need for early detection of disorders.