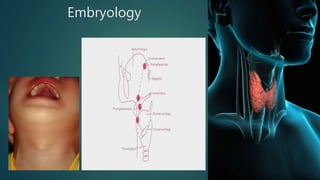
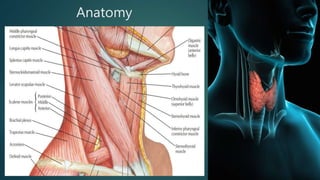
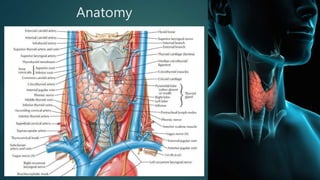
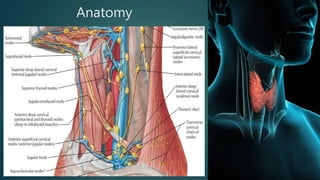
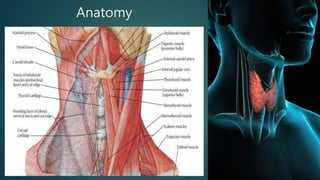
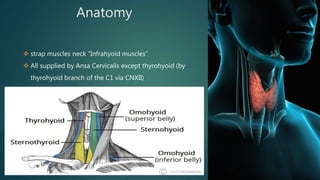
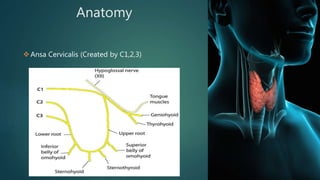
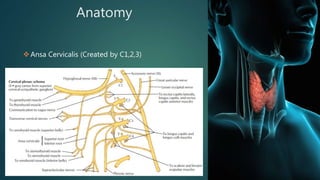
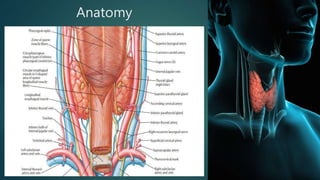
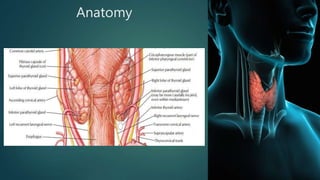
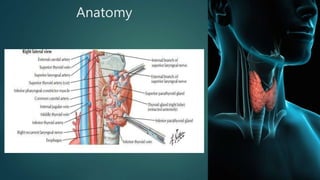
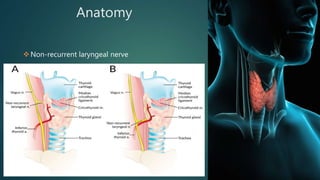
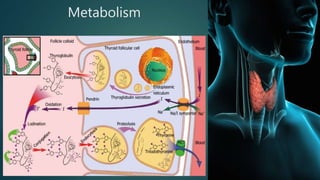
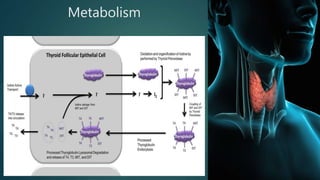
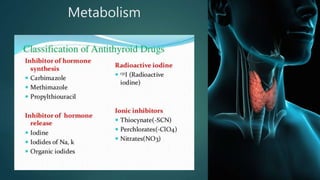
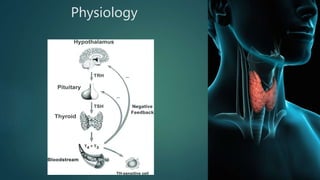
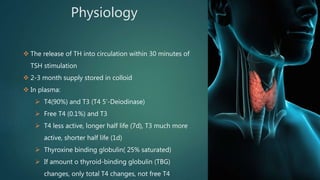
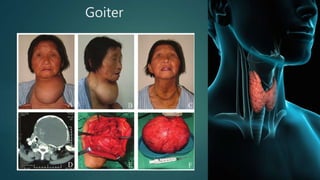
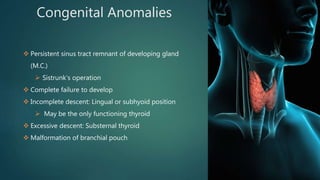
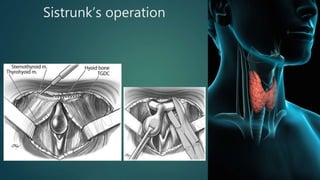
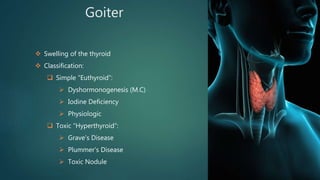
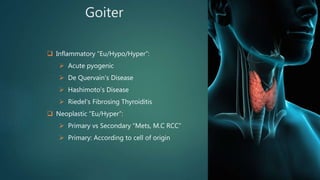
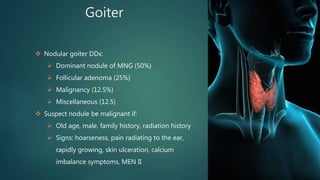
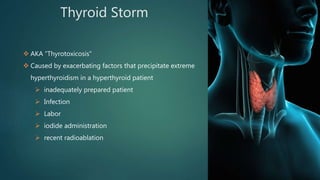
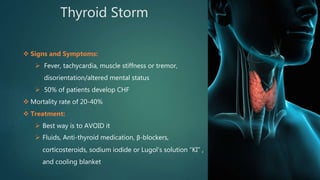
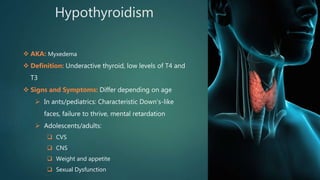
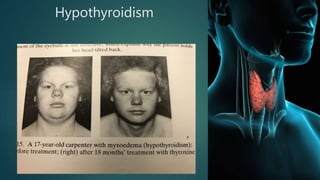
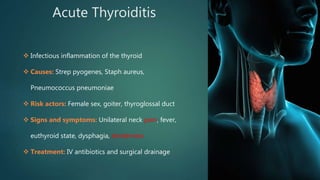
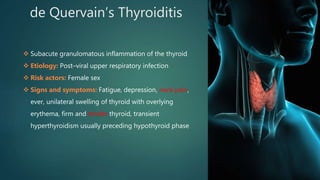
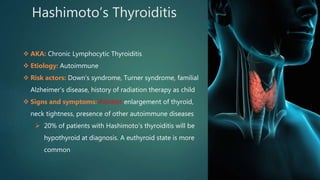
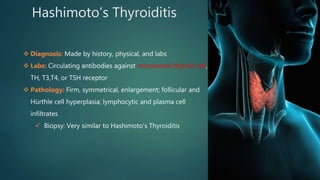
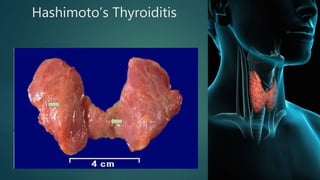
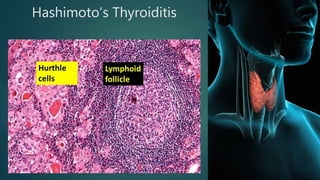
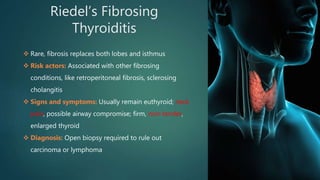
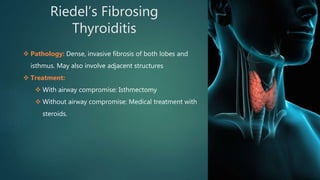
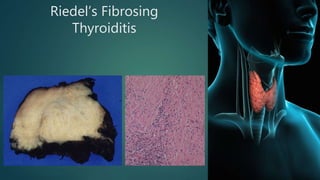
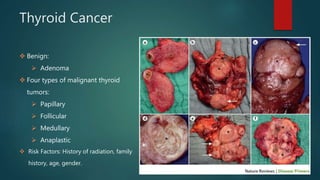
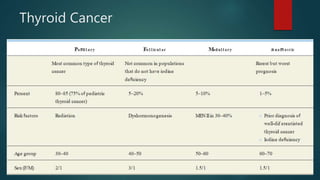
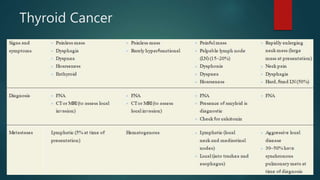
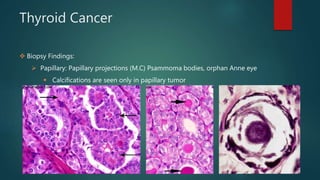
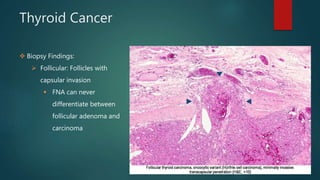
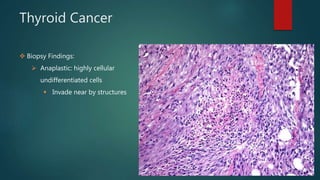
This document provides an overview of the thyroid gland, including its anatomy, embryology, histology, physiology, common diseases and disorders. It discusses topics such as thyroid development, hormone production, hyperthyroidism and hypothyroidism, different types of thyroiditis including Hashimoto's, and thyroid tumors. The key information covered includes the location and blood supply of the thyroid, how it produces thyroid hormones and calcitonin, common signs and symptoms of overactive and underactive thyroid, and descriptions of Graves' disease, multinodular goiter, thyroid storm, and different forms of thyroiditis.