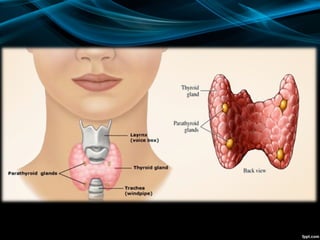
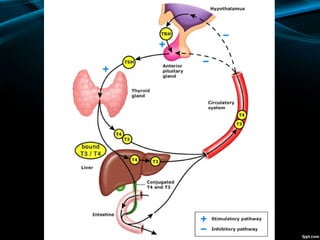
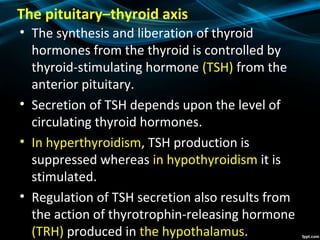
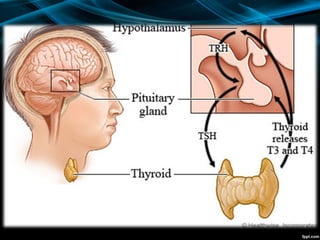
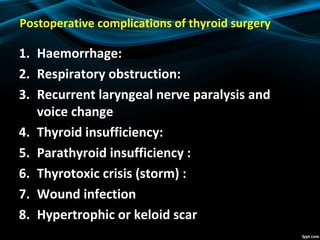
The document discusses the physiology of the thyroid gland and thyroid hormones such as T3 and T4. It describes how the pituitary-thyroid axis controls thyroid hormone production and discusses different types of thyroid enlargement including simple goiter, diffuse hyperplastic goiter, toxic nodular goiter, and Graves' disease. The principles and advantages/disadvantages of different treatment approaches for hyperthyroidism are provided, including anti-thyroid drugs, surgery, and radioiodine therapy. Potential postoperative complications of thyroid surgery are also listed.