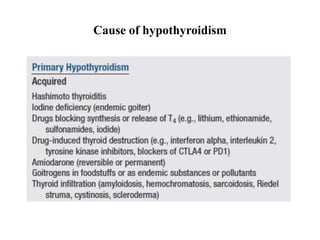
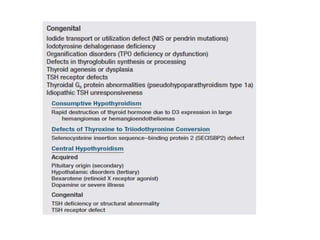
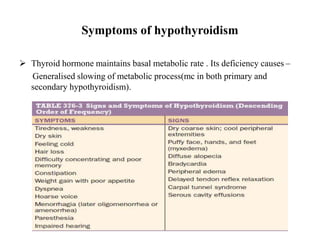
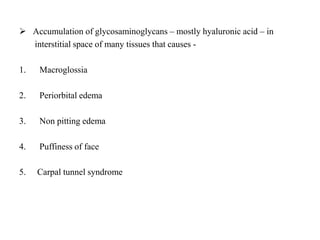
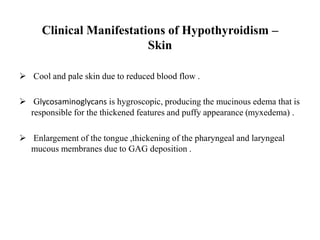
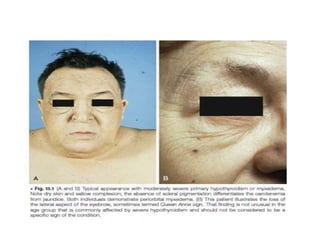
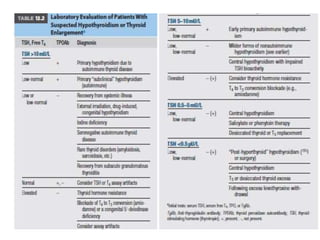
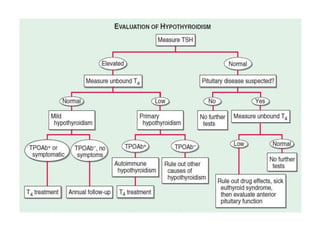
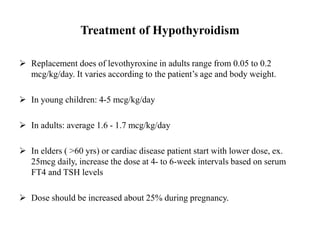
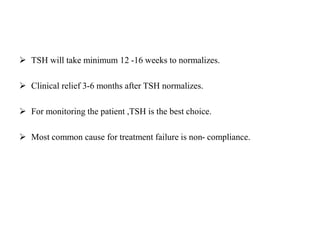
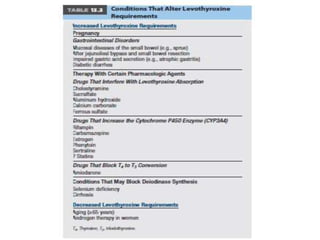
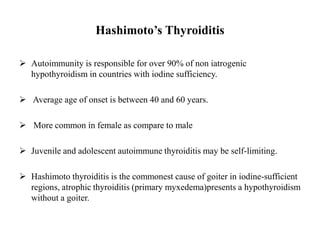
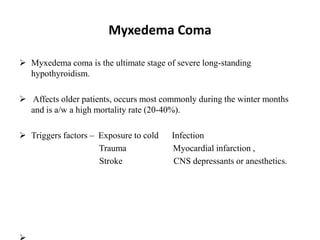
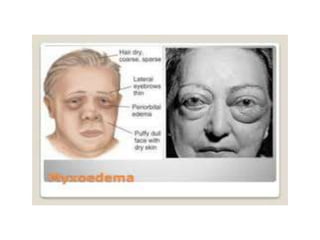
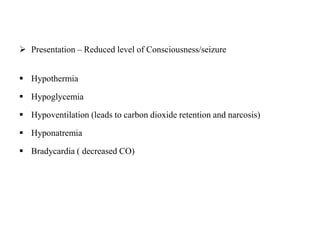
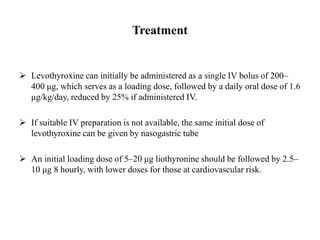
Hypothyroidism is a condition caused by reduced production of thyroid hormones. The main types are primary hypothyroidism due to permanent thyroid damage or failure, and central/secondary hypothyroidism due to pituitary or hypothalamic issues. Hashimoto's disease is the most common cause of primary hypothyroidism. Symptoms include fatigue, dry skin, constipation, weight gain and slowed heart rate. Treatment involves thyroid hormone replacement via levothyroxine. Subclinical hypothyroidism may also be treated depending on risk factors. Hypothyroidism in pregnancy requires careful management to prevent complications. In severe cases, myxedema coma can develop with risk of high mortality and requires urgent