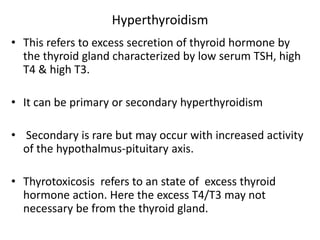
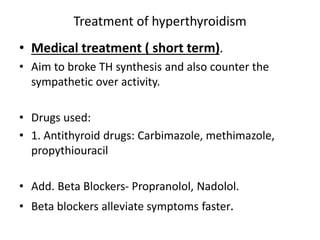
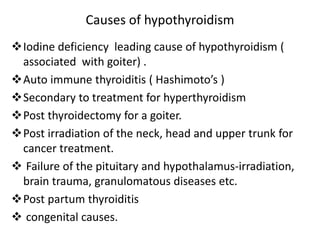
1) The document discusses hyperthyroidism and hypothyroidism, which are conditions caused by abnormal thyroid hormone levels. Hyperthyroidism is caused by excess thyroid hormone production, while hypothyroidism is caused by insufficient hormone production.
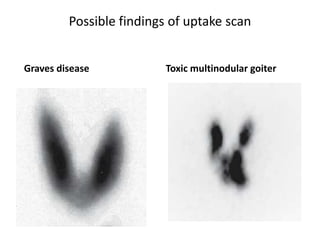
2) Common causes of hyperthyroidism include Graves' disease, toxic multinodular goiter, and toxic adenoma. Hypothyroidism is commonly caused by iodine deficiency, autoimmune thyroiditis, and treatment for hyperthyroidism.
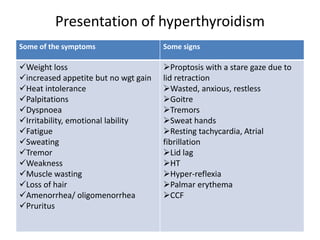
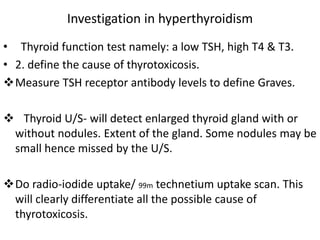
3) Symptoms and signs of the conditions vary but include changes in appetite, weight, and mood. Diagnosis involves thyroid function tests measuring TSH, T4, and T3 levels