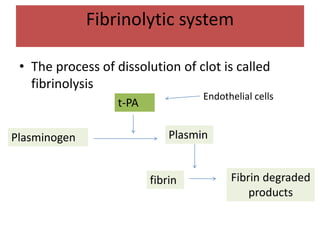
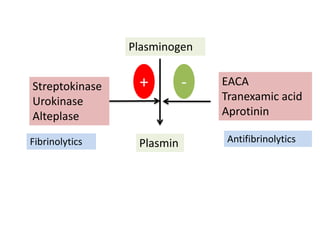
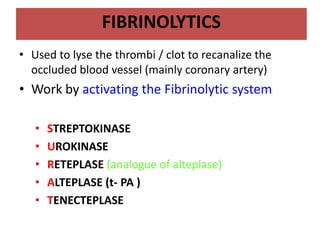
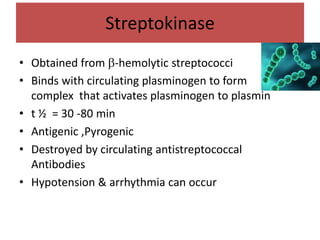
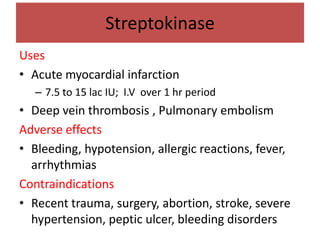
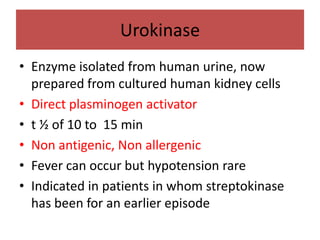
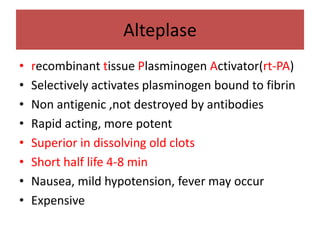
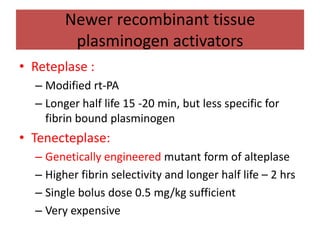
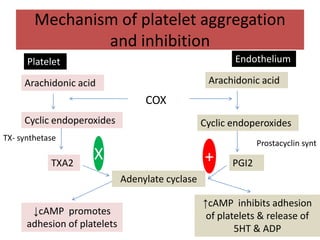
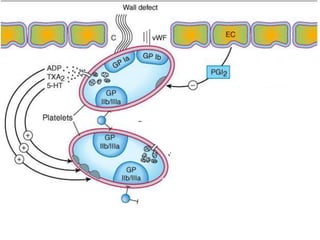
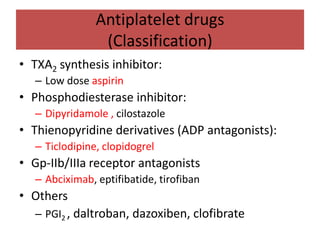
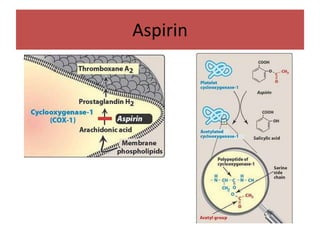
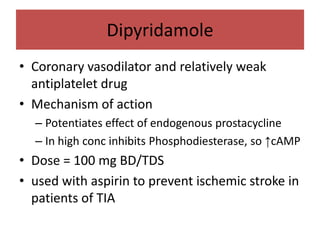
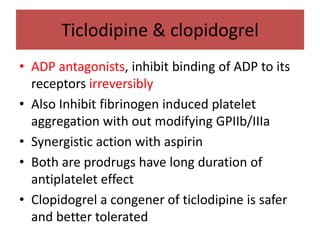
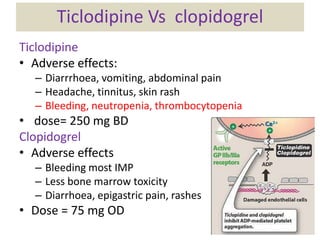
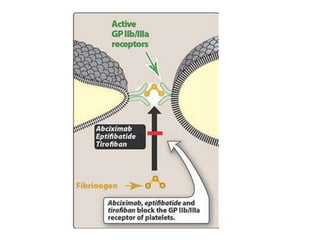
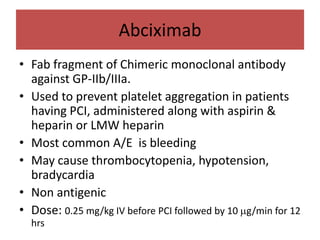
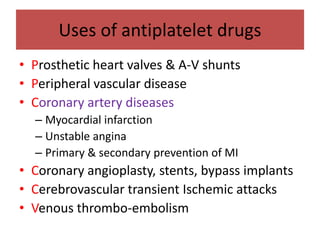
This document summarizes fibrinolytics and antiplatelet drugs. It describes the fibrinolytic system and how fibrinolytics like streptokinase, urokinase, alteplase work to activate plasminogen and lyse clots. Newer fibrinolytics like reteplase and tenecteplase are discussed. Antiplatelet drugs discussed include aspirin, dipyridamole, clopidogrel, abciximab and how they inhibit platelet aggregation by blocking TXA2 synthesis, increasing cAMP, or blocking ADP/GP-IIb-IIIa receptors. Their uses for coronary artery disease and procedures are highlighted.