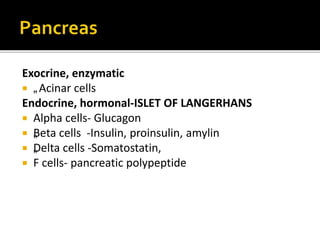
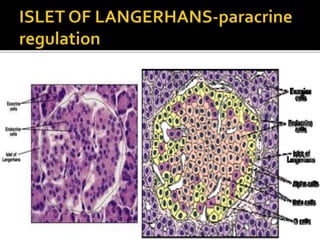
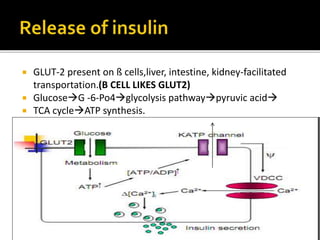
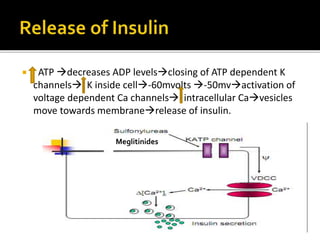
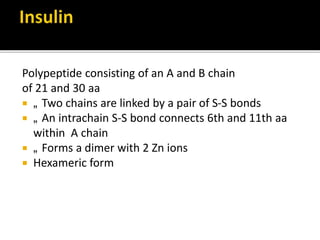
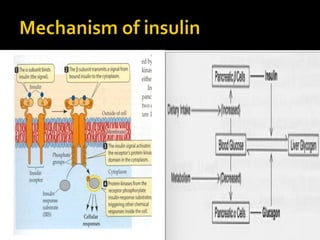
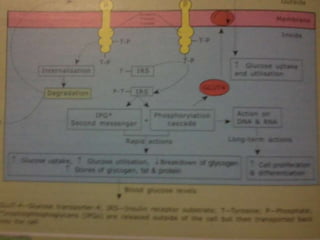
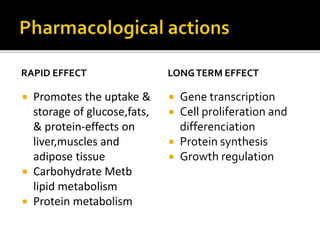
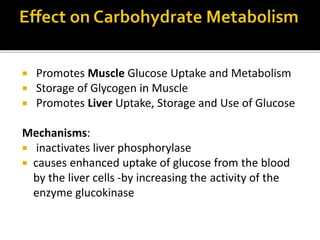
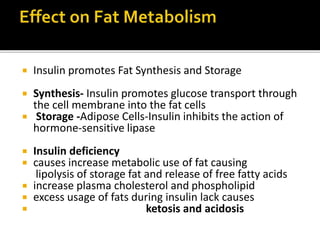
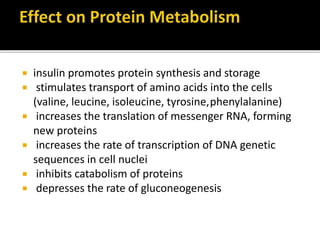
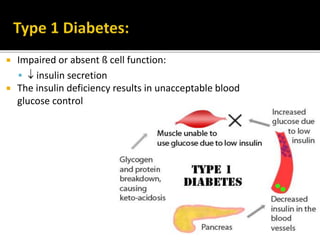
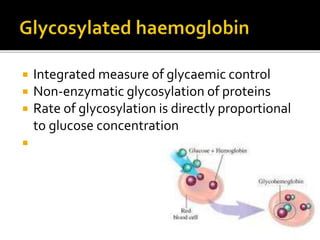
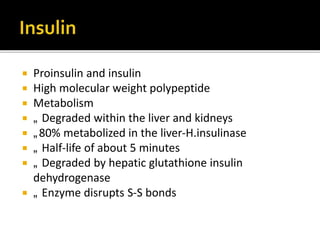
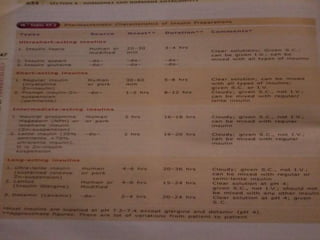
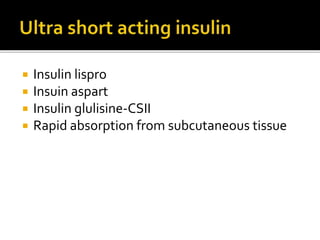
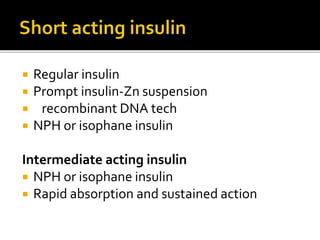
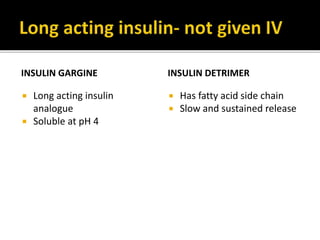
This document discusses the pancreas and its exocrine and endocrine functions. It focuses on the production and regulation of insulin in the pancreatic beta cells. Insulin regulates glucose and lipid metabolism, protein synthesis, and the storage and use of nutrients in tissues. The mechanisms of insulin secretion and action are described. The types and uses of insulin preparations are outlined, as are the complications of diabetes and methods for monitoring glucose control. Other diabetes medications like GLP-1 agonists are also briefly mentioned.