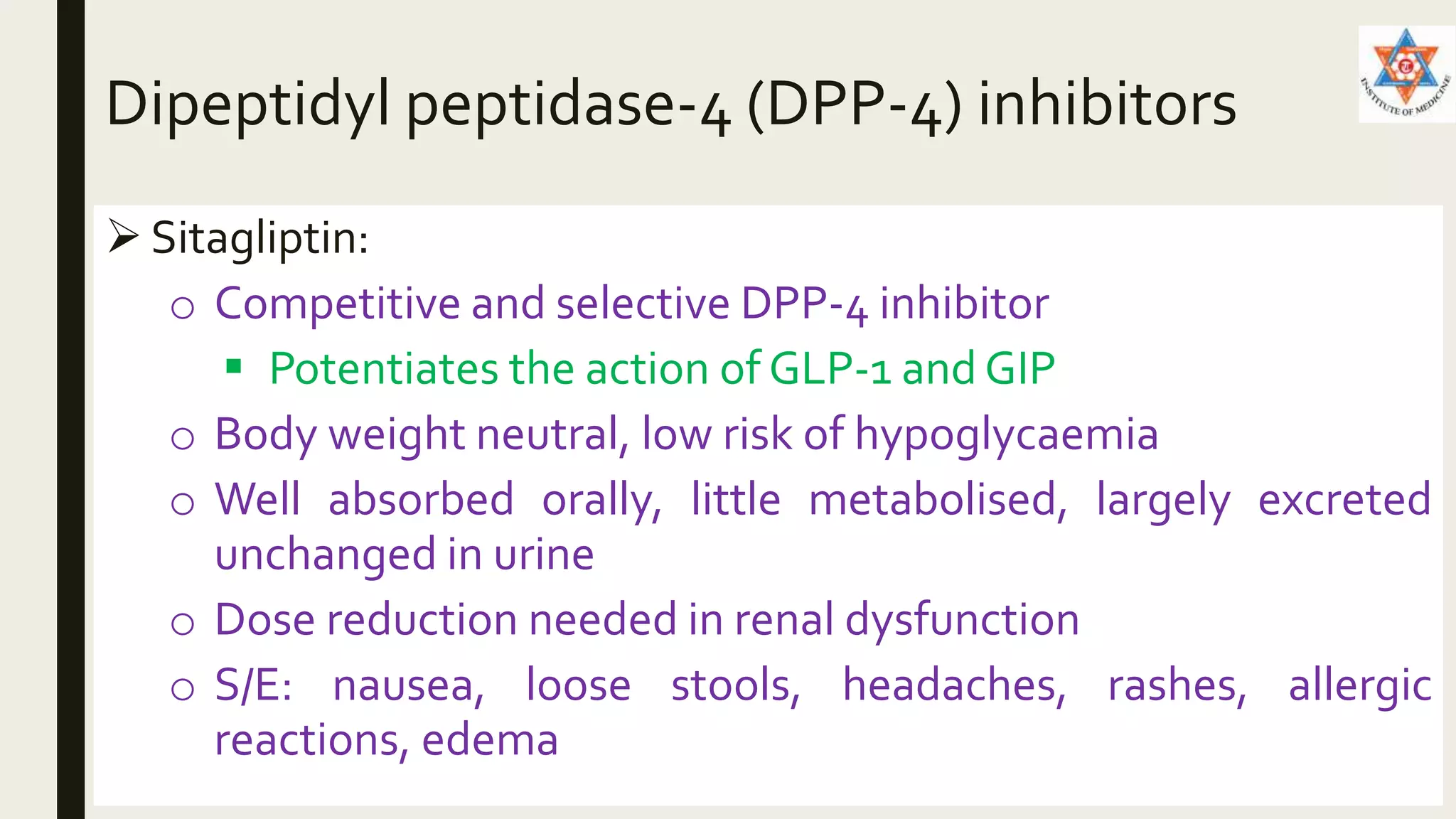
Oral hypoglycemic agents are classified based on their mechanism of action. Sulfonylureas work by blocking potassium channels in pancreatic beta cells, increasing calcium influx and insulin secretion. Meglitinides like repaglinide have a similar quick-acting mechanism. DPP-4 inhibitors like sitagliptin increase GLP-1 and GIP action. Biguanides like metformin activate AMPK, suppressing glucose production and enhancing uptake. Thiazolidinediones like pioglitazone activate PPARγ, enhancing insulin sensitivity. Other agents include alpha-glucosidase inhibitors, amylin analogues, and SGLT2 inhibitors. While effective at lowering blood glucose,