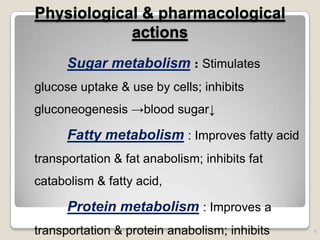
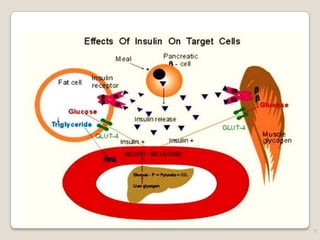
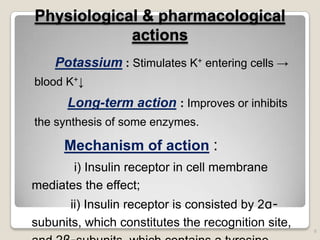
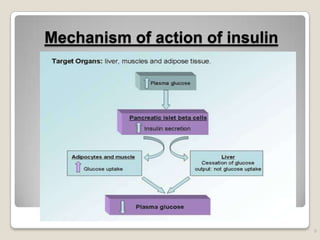
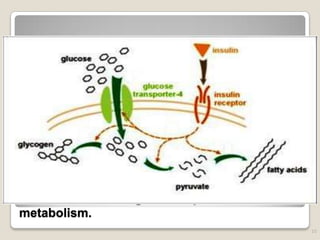
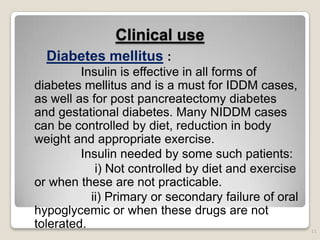
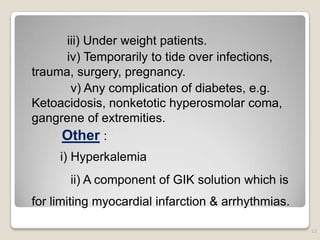
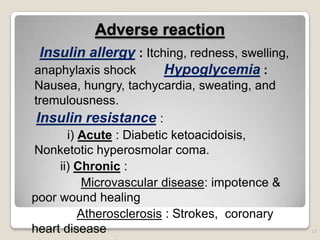
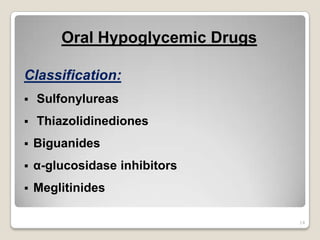
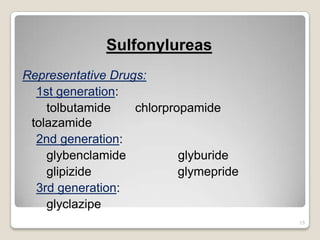
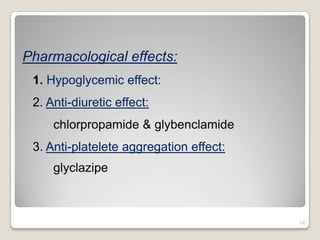
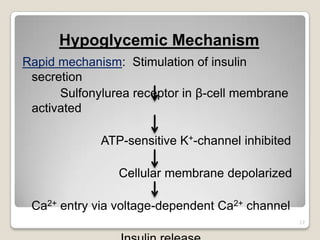
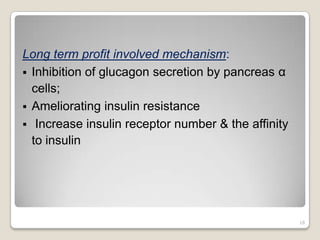
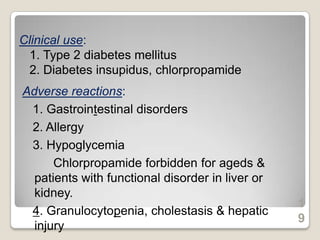
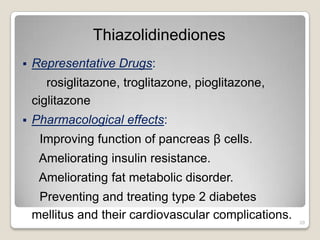
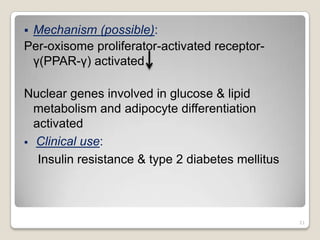
Diabetes mellitus is a metabolic disorder characterized by hyperglycemia. There are two major types: insulin-dependent diabetes mellitus (IDDM) and non-insulin dependent diabetes mellitus (NIDDM). Insulin is secreted by pancreatic beta cells and helps regulate blood sugar levels. It is essential for treating IDDM and sometimes needed for NIDDM. Oral hypoglycemic drugs like sulfonylureas and thiazolidinediones are also used to treat NIDDM by stimulating insulin secretion or improving insulin sensitivity. Both insulin and oral hypoglycemic drugs can cause hypoglycemia as an adverse reaction if not used properly.