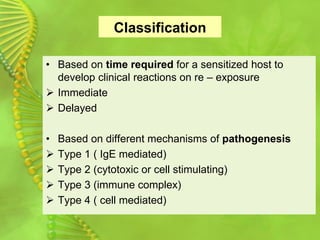
This document discusses the different types of hypersensitivity reactions:
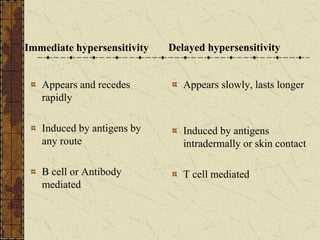
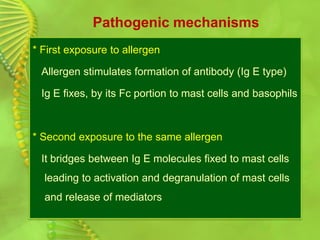
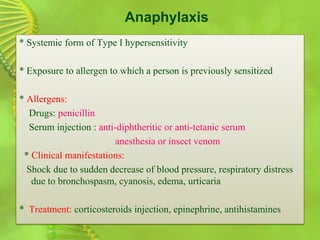
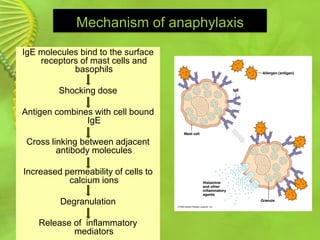
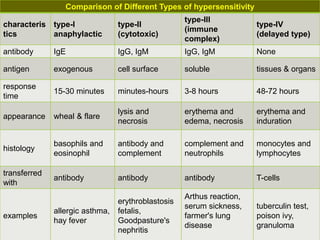
1. Type I reactions are immediate and antibody-mediated, involving IgE. They cause conditions like allergic asthma and anaphylaxis.
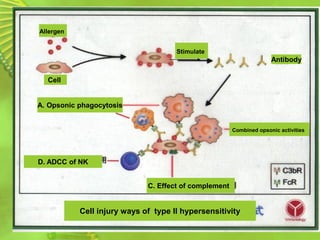
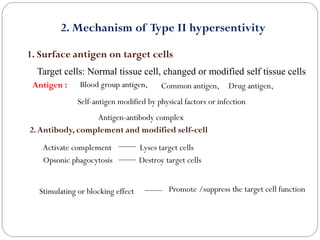
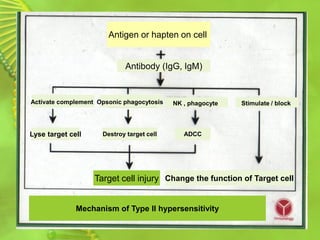
2. Type II reactions are cytotoxic and involve IgG/IgM binding to cell surfaces and activating complement. They can lyse cells.
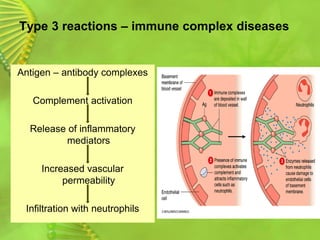
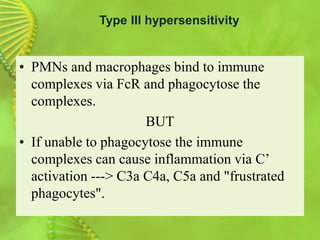
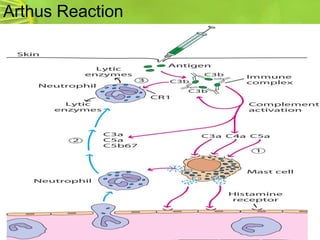
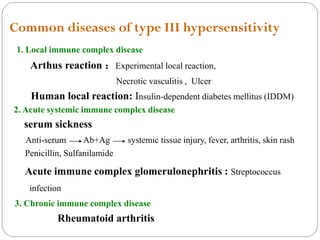
3. Type III reactions involve soluble immune complexes activating complement and causing inflammation. They include serum sickness.
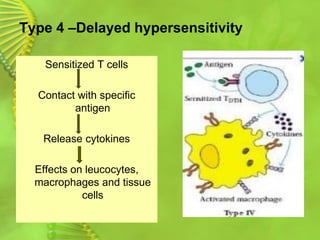
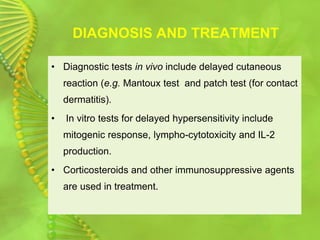
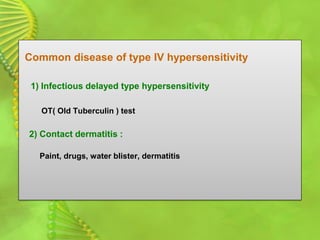
4. Type IV reactions are delayed, cell-mediated responses involving sensitized T cells and cytokines. They cause conditions like contact dermatitis.