This document discusses the different types of hypersensitivity reactions:
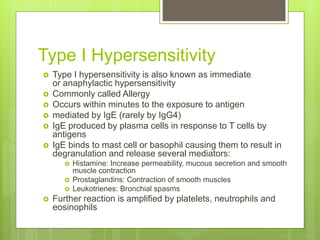
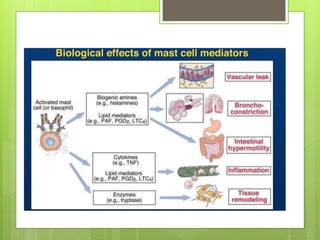
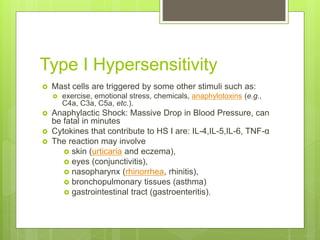
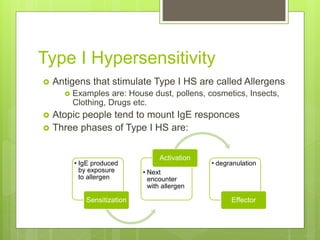
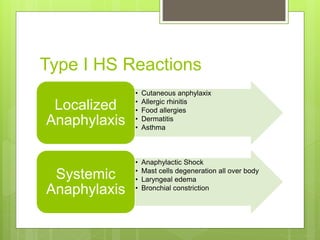
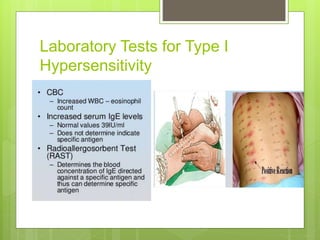
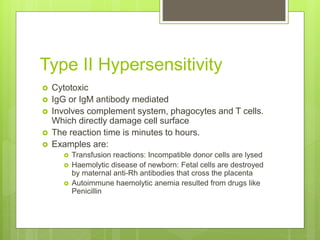
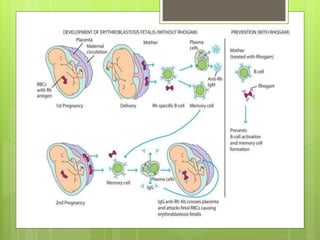
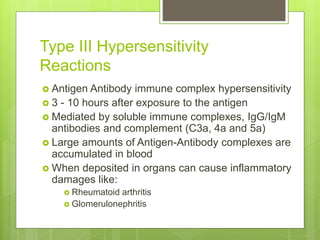
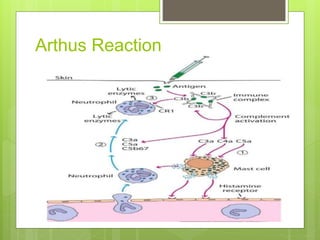
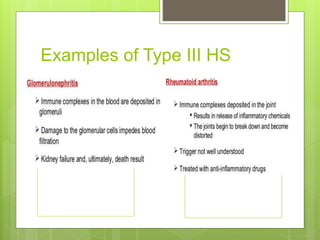
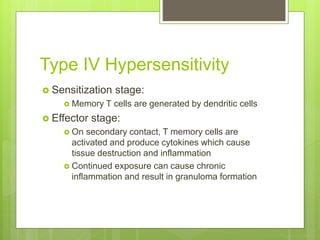
Type I reactions are immediate and anaphylactic, mediated by IgE antibodies binding to mast cells. Type II reactions are cytotoxic and antibody-mediated, directly damaging cells. Type III reactions involve immune complex deposition causing inflammation. Type IV reactions are delayed and T cell-mediated, causing localized reactions where antigen is present. The types are distinguished by the mechanisms and timescales involved. Hypersensitivity reactions can cause issues in various tissues and organs.