The document summarizes different types of hypersensitivity reactions:
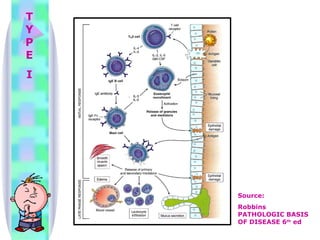
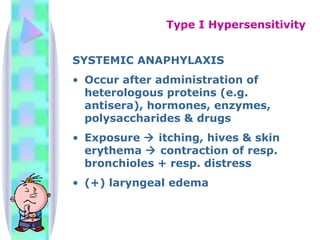
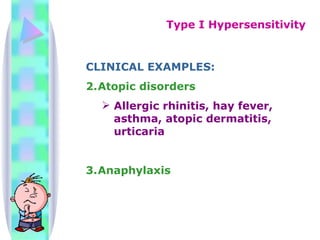
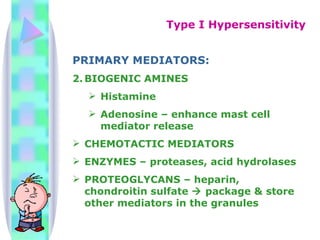
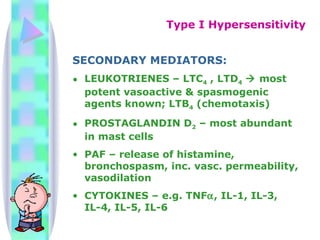
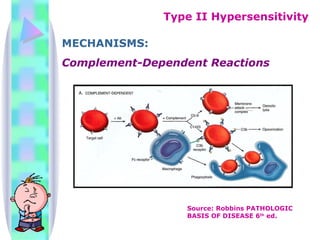
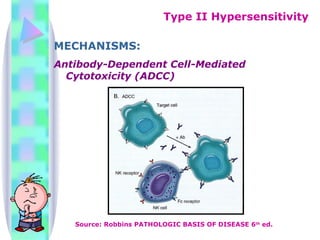
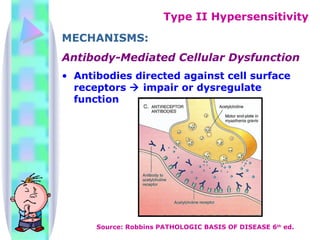
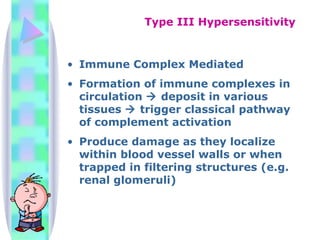
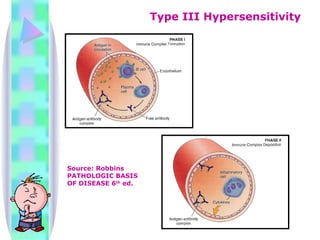
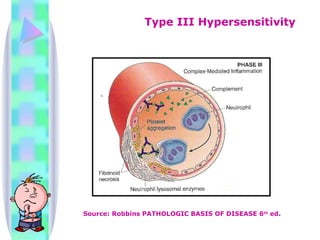
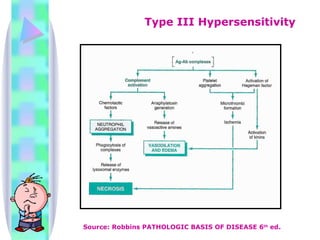
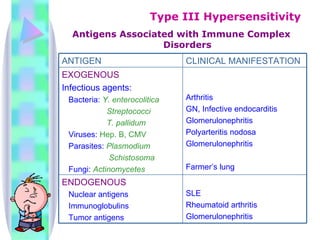
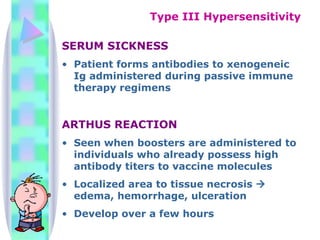
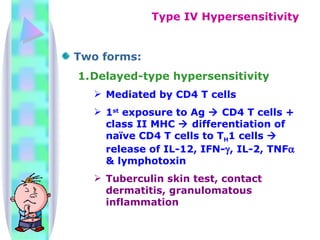
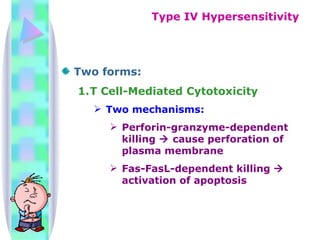
Type I reactions are immediate and mediated by IgE antibodies. They cause conditions like allergic rhinitis and anaphylaxis. Type II reactions are caused by IgG and IgM antibodies binding to cells, activating complement and causing cell lysis. Type III reactions involve immune complexes forming in circulation and depositing in tissues, activating complement and causing damage. Type IV reactions are cell-mediated, initiated by sensitized T cells, and cause delayed hypersensitivity responses and cytotoxic killing of infected cells.