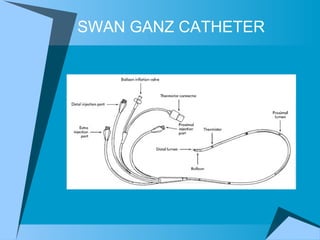
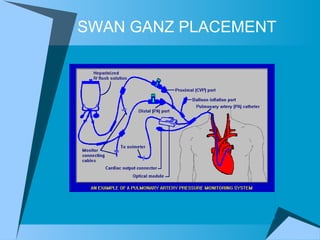
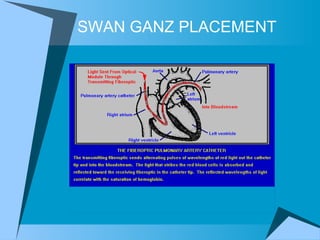
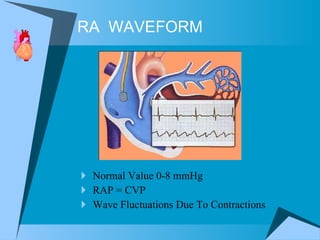
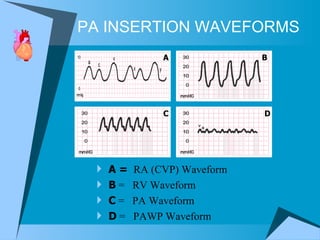
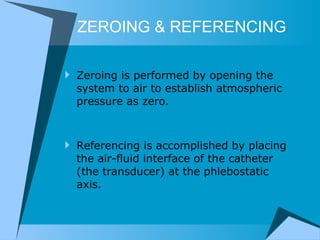
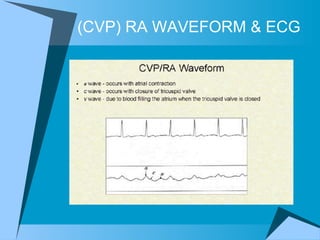
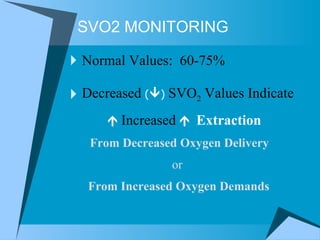
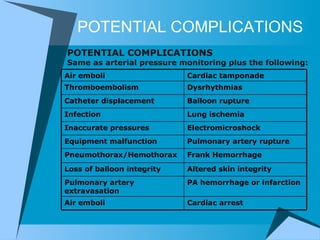
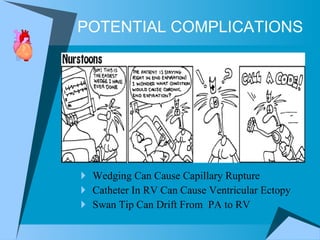
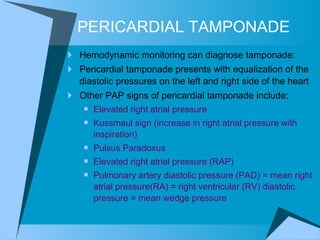
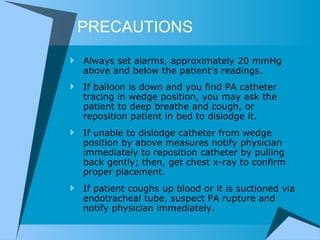
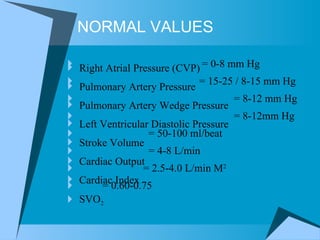
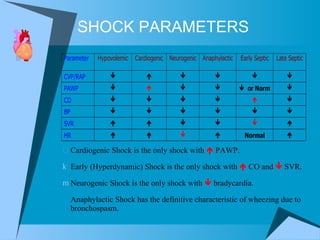
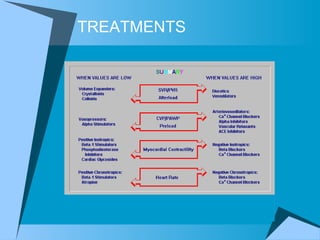
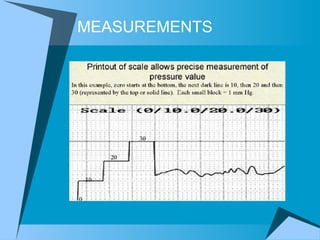
Hemodynamic monitoring measures factors that influence the force and flow of blood in order to aid in diagnosing, monitoring, and managing critically ill patients. It involves using pulmonary artery catheters and transducers to obtain pressures and other cardiovascular measurements that provide information on conditions like shock states and help guide treatment decisions. Potential risks and complications require careful use of these monitoring techniques in appropriate clinical situations.